By La Rissa Vasquez, Neurobiology, Physiology & Behavior ‘23
Author’s Note: In this paper, I analyze autopsy reports conducted on deceased COVID-19 patients and supply a breakdown of the body’s immune response. The purpose of this paper is to provide a more generalized synopsis of how the body is affected by the virus from the onset of infection to the escalating factors that contribute to cause of death. COVID-19 and SARS-CoV-2 are referenced countless times throughout this paper, but they should not be used interchangeably. The name of the pathogenic virus is “Severe Acute Respiratory Syndrome Coronavirus 2” (SARS-CoV-2), and the name of the illness is called COVID-19 and is the common usage in forms of discussion. This paper only scratches the surface of the virus’s complexity and its effects upon the body and societies around the world.
Introduction
On December 31, 2019, the first case of the novel coronavirus was reported in Wuhan, China [1]. The first case of the virus reported in the United States was on January 22, 2020 [2]. Within 22 days, the Coronavirus had traveled across the Pacific to wreak havoc upon countries woefully unprepared. Within a year, COVID-19 has managed to bring some of the most powerful countries in the world to heel. Economies and healthcare systems across the world continue to be devastated by an adversary only 60 to 140 nanometers in diameter [3]. On February 11, 2020, the International Committee on Taxonomy of Viruses (ICTV) formally identified the virus as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). On March 11, 2020, the World Health Organization classified COVID-19 as a worldwide pandemic and global health crisis [4]. As of May 2021, the CDC has confirmed that the U.S. has over 32 million cases. Healthcare systems across the nation and around the world are overwhelmed by the number of infected patients. Many of them perish due to either a lack of resources or accurate and efficient testing.
SARS-CoV-2 Viral Pathogenesis
Humans have two levels of immunity. Innate immunity is the body’s first line of contact and defense against invading pathogens. Adaptive immunity learns and remembers how to effectively target and eliminate these pathogens.
Innate Immunity
Our innate immune system is composed of barrier tissues and cells specialized for defense against pathogens [5]. Barrier tissues are the first line of defense, and inside barrier tissues reside sentinel cells, which are capable of consistently recognizing repeated exposure to pathogen associated molecular patterns (PAMPs). The sentinel cells release proinflammatory mediators like cytokines, chemokines, or histamines and circulate within the blood vessels inviting more immune cells from the surrounding tissue into the bloodstream [5]. Cells such as neutrophils or monocytes differentiate into macrophages and migrate from the bloodstream and phagocytose (eat) the pathogens. Neutrophils will undergo programmed cell death, referred to as apoptosis. Macrophages will continue to phagocytose the rest of the pathogens and restore homeostasis by consuming the dead neutrophils [5].
Infection occurs when these viral pathogens in respiratory droplets from a sneeze or a cough enter a person’s mouth, nose, or eyes and attach to the ACE-2 receptors in the nose, throat, and especially the lungs. Like any virus, SARS-CoV-2 cannot replicate on its own and instead hijacks the body’s own cellular machinery. The virus inserts its own genetic information into the host cell to produce more copies of itself until the cell bursts and dies, spreading more of the virus around the body to infect more cells [6]. Infection of the host cell consists of the following five steps: attachment, penetration, biosynthesis, maturation, and release. Once a virus binds to host receptors (attachment), it enters host cells via endocytosis or membrane fusion (penetration). Once the viral contents are released inside the host cells, viral RNA are transported by protein molecules in the host cell’s cytoplasm and travel into the nucleus for replication via the nuclear pore complex (NPC). Viral mRNA then makes viral proteins (biosynthesis). Lastly, novel viral particles are made (maturation) and released [7]. This innate immune response is not as effective against SARS-CoV-2 due to the strength of the various proteins displayed in Figure 1, an ultrastructural morphology rendering, provided by the Centers for Disease Control and Prevention (CDC) Image Library on February 10 [8].
Figure 1
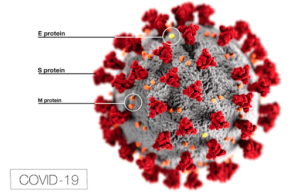
The SARS-CoV-2 virus contains “M (membrane), S (spike), E (envelope), and N (nucleocapsid)” proteins, which envelop the virion and act as a defensive shield [9]. The S or Spike viral surface protein, which consists of two subunits, S1 and S2, binds to the angiotensin converting enzyme 2 (ACE2) receptors of the host cells [7]. The primary role of ACE2 is the breakdown of the angiotensin II (ANG II) protein into molecules that neutralize its harmful effects. ANG II is responsible for increased inflammation and death of alveolar cells in the lungs, which reduces oxygen uptake. When the S (spike) protein of SARS-CoV-2 binds to the ACE2 receptors, they inhibit ACE2 from doing its job of regulating ANG II, allowing ANG II to freely damage tissue in the lungs. These ACE2 receptors are naturally present on the surface of the lung’s epithelial cells and other organs throughout the body, but the virus’ S protein uses these receptors to penetrate the cell membrane and replicate inside host cells. The N (nucleocapsid) protein is another viral surface protein of SARS-CoV-2, which inhibits interferons (IFN1 and IFN-β) responsible for cytokine production [10]. But if the signals for regulating proinflammatory response are disrupted by the pathogen’s surface proteins, the innate immune response becomes hyperactive and self-destructive. A malfunctioning innate immune response also compromises an adequate adaptive immune response [9].
Adaptive Immunity
Adaptive immunity consists of B-cell and T-cell responses. B-cells produce antibodies to trigger an immune response, while T-cells actively target and eliminate infected cells.
B-Cell Response
The innate immune response is not particularly equipped to combat pathogens that are especially complex and vicious because the innate immune response is non-specific and will attack anything it identifies as an invader. The adaptive immune response can target pathogens more precisely and powerfully by using proteins called antibodies, which are produced by B-cell lymphocytes that bind to antigens on the surface of pathogens [5]. Adaptive immunity can more efficiently handle foreign pathogens, like a virus, because antibodies can see through the debris of proteins and dead cells left by the cytokine storm. Antibodies uniquely bind to antigens, acting as a beacon for the adaptive immune response to converge on the invading pathogen [5]. More importantly, adaptive immunity has memory and learns how to become more effective by retaining its response to pathogens so that it can be even quicker at eliminating them after repeated exposure [5]. Widespread pandemics like COVID-19 occur because of a lack of protective antibodies in populations that have never been exposed to or vaccinated against the specificity of SARS-CoV-2 [5]. Figure 2 depicts the four ways in which antibodies attack pathogens: neutralization, complement fixation, opsonization, and antibody dependent cellular cytotoxicity.
Figure 2
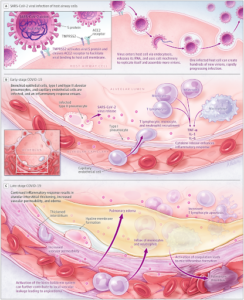
Figure 2 – “Immunopathogenesis of Coronavirus Disease 2019 (COVID-19)” [3].
Neutralization is the process by which antibodies immediately bind to the surface antigens of a pathogen and block their S protein from attaching to the receptors of healthy cells, thereby neutralizing the virus’ ability to attach and insert its genetic information. Complement fixation occurs when antibodies are responsible for inviting complement proteins to bind to the antigens of the pathogen. This process coats the pathogen in attack proteins that can either initiate the complement cascade leading to cell lysis, the breakdown of the cell, or it can induce the third stage, opsonization. During opsonization, proteins called opsonins bind to the invading pathogen, acting as markers for phagocytotic cells like macrophages to identify and consume the pathogen. Lastly, antibody dependent cellular cytotoxicity (ADCC) is the process by which antibodies recognize the antigen of a pathogen and signal for natural-killer cells (NK cells) to release cytotoxic molecules which kill off the virally infected cell [5].
T-Cell Response
T-cell lymphocytes are produced by the bone marrow and mature in the thymus. They form the basis of cellular immunity because they directly attack foreign pathogens. Consequently, they are more effective than innate immune or B-cell responses at targeting intracellular pathogens like viruses [5]. Antibodies can get distracted by viral particles and proteins, so they rely on the blind T-cell lymphocytes to ignore the surrounding virus particles and eliminate the infected host cell at the source. As naive T-cells circulate the lymph nodes and spleen, they express T-cell receptors (TCR) that recognize cell surface peptides (antigens) attached to major histocompatibility complex (MHC) molecules on the surface of a specific pathogen. These surface MHC proteins tell the T-cells where to attack [5]. The dendritic cells work to activate the adaptive immune response by ingesting viral proteins and turning them into cell surface peptides that bind to MHC molecules, forming peptide-MHC complexes. The TCR of naive T-cells recognize the peptide-MHC complexes and activate the T-cell. For T-cells to become active, they also need to bind to proteins from the dendritic cell via co-simulation. They then undergo clonal expansion and differentiate into effector T-cells [5]. Effector T-cells are also referred to as cytotoxic T lymphocytes (CTLs). They travel through the body to hunt down peptide-MHC presenting pathogens and kill the infected cells by releasing cytotoxic molecules [5].
The adaptive immune response is stimulated by the recognition of pathogen-associated molecular patterns (PAMPs). Within 1-2 weeks after infection, the B-cells produce antibodies while T-cells simultaneously increase proinflammatory cytotoxic molecules in a forceful attempt to eliminate the virus [7]. The uptick in Interleukin cytokines abbreviated as IL-1, IL-6, IL-8, and so on, flood the body with proinflammatory substances, which “chronically increase the stimulation of T-cells, resulting in a cytokine storm and T-cell exhaustion” [9]. T-cell exhaustion not only means that the virus is overwhelming the body’s antibodies but also draining the strength of the T-cell’s ability to eliminate the virus at the source of infected host cells. SARS-CoV-2 is a “high-grade chronic viral infection because it decreases the responsiveness of T-cells leading to a decreased effector function and lower proliferative capacity” [9]. T-cell exhaustion is also linked to an increase in inhibitory receptors that can initiate apoptosis in T-cells. This results in the destruction of T-cells and their co-receptors, further suppressing the T-cells, as well as B-cells and NK cells, all of which are white blood cells (lymphocytes). Thus, explaining the general lymphopenia (the lack of lymphocytes) observed in severe COVID-19 cases and the increased number of cytokines [9]. Viral entry and attachment to ACE2 receptors trigger a vicious cycle of both innate and adaptive immune responses, mounting an intense attack by secreting proinflammatory substances that invite more lymphocytes to try and kill the virus. This releases more cytokines and chemokines [11]. The downregulation of the ACE2 enzyme results in a cascade of chemical reactions that lead to further inflammation and destruction of cells, weakening and damaging the body’s own immune response.
pathologies of a pandemic:
COVID-19 Autopsies
Once the SARS-CoV-2 attaches to alveolar type II cells, it propagates within the cells. Most viral particles cause apoptosis, releasing more self-replicating pulmonary toxins. Figure 3 displays normal ACE2 receptors located in the type II pneumocytes. Healthy alveoli are unobstructed to allow efficient diffusion of oxygen and carbon dioxide with red blood cells.
Figure 3
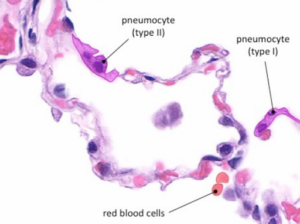
Figure 3 – “Type I pneumocytes are very thin in order to mediate gas exchange with the bloodstream (via diffusion). Type II pneumocytes secrete a pulmonary surfactant in order to reduce the surface tension within the alveoli” [12].
In contrast to Figure 3, Figure 4 shows the histopathology of alveolar damage (A) and inflammation (B) of the epithelial cells. As the epithelial cells detach from the alveolar wall the alveoli structures collapse and no longer inflate making it hard for patients with severe cases of COVID to breathe [13]. This results in diffuse alveolar damage with fibrin rich hyaline membranes and hemorrhages in the lungs [13]. The histopathology also detected multinucleated cells that lead to pulmonary fibrosis (scarring in the lungs). Infected cells are “abnormally large and often polynucleated cells showing a large cytoplasm with intense staining for the COVID-19 RNA probe” [13]. The viral Spike protein is also largely detected in the histopathology of COVID cases (C). The nuclei of Spike-positive cells appear an intense red stain and have abnormally enlarged cytoplasts (panel h) [13].
Figure 4
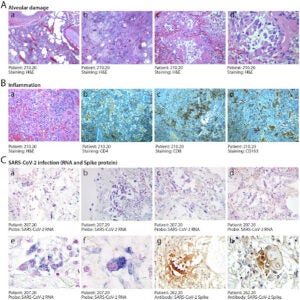
Figure 4 – “Histopathological evidence of alveolar damage, inflammation and SARS-CoV-2 infection in COVID-19 lungs” [13].
The cellular destruction detected in the histopathology is macroscopically reflected in the physical damage of lung tissue displayed in Figure 5.
Figure 5
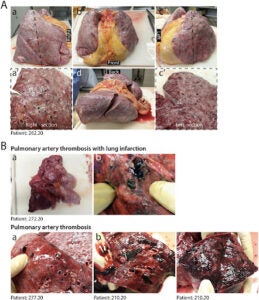
Figure 5 – “Macroscopic appearance of COVID lungs” [13].
In all pathological examinations of patients that died of COVID, their lungs sustained macroscopic damage [13]. Severe cases of COVID reveal congested and firm lungs (A) with “hemorrhagic areas and loss of air spaces (a’, c’)” [13]. As the virus ravages the body, some patients rapidly deteriorate and develop severe inflammation and clotting in the lungs (B) which shows “the thrombosis of large pulmonary vessels, often with multiple thrombi and in one case determining an extensive infarction in the right lobe (Fig. 5B panels a and b)” [13]. The lung’s architecture crumbles as cells lose their integrity and continue to die, thus resulting in the development of Acute Respiratory Distress (ARDS). ARDS develops in about 5% of COVID-19 patients, and of all the infected, the mortality rate remains around 1 to 2% [14]. Autopsies are beginning to reveal that rather than a singular cause of death, many factors seem to be responsible for higher mortality rates in patients that develop critical cases of COVID-19.
The fallout from the hyperactive immune response disrupts regular oxygen diffusion from the alveoli into the capillaries and consequently to the rest of the body. This commonly leaves fluid and dead cells, resulting in pneumonia, a condition in which patients experience symptoms such as coughing, fever, and rapid or shallow breathing [14]. If oxygen levels in the blood continue to drop, patients rely on breathing assistance by a ventilator to forcefully push oxygen into damaged lungs “riddled with white opacities where black space—air—should be” [14]. The presence of opacities in the lungs indicate the development of pneumonia into ARDS, which was found in the autopsy of a 77-year-old man with a history of comorbidities, including hypertension and the removal of his spleen (splenectomy) [15]. The decedent exhibited chills and an intermittent fever but no cough for 6 days. On March 20, 2020, emergency medical services responded to a call, stating that the deceased was experiencing weakness, fever, and shortness of breath. In route to the hospital, the decedent went into cardiac arrest and died shortly after reaching the hospital [15]. A postmortem nasopharyngeal swab was administered and came back positive for SARS-CoV-2.
|
Figure 6 |
Figure 7 |
 |
 |
| Figure 6 – Normal chest X-Ray of healthy lungs [16]. | Figure 7 – “Lesion segmentation results of three COVID-19 cases displayed using the software post-processing platform” [17]. |
Figure 7 shows opacities in the CT “of typical COVID-19 infection cases at three different infection stages: the early stage, progressive stage, and severe stage” [17]. Figure 7 highlights these opacities in red, which appear to intensify and cover more of the lung CT as the virus increases in severity (a-c). Patient 4 (c) exhibits what medical examiners refer to as a “complete whiteout” of the lungs. Indicating reduced air flow, whereas the normal scan of healthy lungs (Figure 6) has a black background, representing the transparency of free and unrestricted airflow.
The postmortem radiography of the deceased 77-year-old man showed “Diffuse, dense bilateral airspace consolidations (complete “whiteout”)” [15]. In most cases of severe COVID-19 “the greatest severity of CT findings is visible around day 10 after the symptom onset. Acute respiratory distress syndrome is the most common indication for transferring patients with COVID-19 to the ICU” [18].
ARDS in connection to SARS-CoV-2 was first documented in Wuhan, Hubei, China in December 2019 with over 90,000 deaths associated with organ dysfunction, particularly progressive respiratory failure and the formation of blood clots resulting in the highest mortality rates [19]. Another autopsy from Hamburg, Germany conducted on the first 12 documented consecutive cases of COVID-19 related deaths revealed that there was not only profuse alveolar damage in 8 out of the 12 patients but also a high rate of clotting resulting in death. 75% of patients that died were males within an age range of 52 to 87 years and 7 out of 12 patients autopsied (58%) presented venous thromboembolism, as displayed in Figure 7. A pulmonary embolism was the direct cause of death in 4 of the deceased [20].
Figure 8
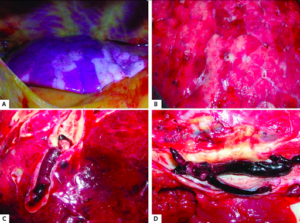
Figure 8 – “Macroscopic autopsy findings: A. Patchy aspect of the lung surface (case 1). B. Cutting surface of the lung in case 4. C. Pulmonary embolism (case 3). D. Deep venous thrombosis (case 5)” [20].
The formation of clots results in pulmonary vasoconstriction, or the constriction of arteries and halting of blood delivery to the arteries and capillaries in the lungs. Blood cannot travel to the lungs, so oxygen levels drop. As a result, a cytokine storm from our hyperactive immune system occurs, destroying the alveolus and the endothelium and causing clots to form. Smaller clots come together and form a fatal giant blood clot, or the clots can break apart and travel to other parts of the body, causing a blockage and inadequate blood supply to organs or other parts of the body [19]. If the blood supply to fingers, toes, and other extremities is cut off by a clot, it is referred to as ischemia and often results in the amputation of digits and appendages once the flesh begins to die [19].
When SARS-CoV-2 enters the alveolar cells in the lungs via the ACE2 receptors, it can directly attack organs and indirectly cause damage to other organs by triggering a hyperactive immune response (cytokine storm). When the viral particles trigger a cytokine storm, they cause further inflammation of the lungs resulting in plummeting oxygen levels and the formation of blood clots in the arteries (arterial thrombosis).
Conclusion
SARS-CoV-2 is a multi-organ scourge, but it primarily attacks the lung by first attaching its spike protein to the host cell’s ACE2 receptors. This prevents the lungs from regulating their function because it inhibits ANG II protein breakdown, causing increased alveolar damage and inflammation of the lungs. The virion proteins create proinflammatory responses in the innate immune response and compromise an effective adaptive immune response. As the virus progresses the number of neutrophils from the innate immune response increase while the number of helpful lymphocytes (T-cells and B-cells) decrease. The ACE2 receptors overstimulate the innate and adaptive immune response to produce more proinflammatory molecules to eliminate the virus, thus causing more destruction to the body and its immune response. Autopsies of COVID-19 victims show ongoing cellular death and collapse of the respiratory system caused by inflammation and alveolar damage that eventually develop into ARDS. Extreme inflammation induced by the immune response causes difficulties in breathing and clotting in the lungs. Radiography of progressive stages of COVID identify opacities in lung CTs indicating obstructed airways and alveolar deterioration. Postmortem examinations reveal gross destruction of the lung tissue, such as pulmonary artery thrombosis, vasoconstriction, lung infarction, or pulmonary embolism. Progressive organ and respiratory failure and abnormal clotting are all contributing factors to the cause of death in the most severe cases of COVID-19.
SARS-CoV-2 efficiently exploits weaknesses not only within our innate and adaptive immune systems across sex, age, race, and ethnicity, but it also exploits weaknesses within our societies. The etymological origins of Pandemic are rooted in pandēmos , which is Greek for ‘all’ (pan)+ ‘people’ (demos). When simplified, pandemic literally means “all people” but the priorities of leadership across the world reveal that not all people suffer the burden of this pandemic equally. Regarding the United States’ approach to the pandemic, this quote from the Atlantic’s article “Why Some People Get Sicker Than Others” is sufficient; “the damage of disease and a global pandemic is not a mystery. Often, it’s a matter of what societies choose to tolerate. America has empty hotels while people sleep in parking lots. Food is destroyed every day while people go hungry. Americans are forced to endure the physiological stresses of financial catastrophe while corporations are bailed out. With the coronavirus, we do not have vulnerable populations so much as we have vulnerabilities as a population. Our immune system is not strong” [21].
References:
1. Fan, Jingchun, Xiaodong Liu, Weimin Pan, Mark W. Douglas, and Shisan Bao. “Epidemiology of Coronavirus Disease in Gansu Province, China, 2020.” Emerging Infectious Diseases 26, no. 6 (2020): 1257-265. doi:10.3201/eid2606.200251.
2. Stokes, Erin K., Laura D. Zambrano, Kayla N. Anderson, Ellyn P. Marder, Kala M. Raz, Suad El Burai Felix, Yunfeng Tie, and Kathleen E. Fullerton. “Coronavirus Disease 2019 Case Surveillance — United States, January 22–May 30, 2020.” MMWR. Morbidity and Mortality Weekly Report 69, no. 24 (2020): 759-65. doi:10.15585/mmwr.mm6924e2.
3. Wiersinga, W. Joost, Andrew Rhodes, Allen C. Cheng, Sharon J. Peacock, and Hallie C. Prescott. “Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19).” Jama 324, no. 8 (2020): 782. doi:10.1001/jama.2020.12839.
4. “Naming the Coronavirus Disease (COVID-19) and the Virus That Causes It.” World Health Organization. Accessed May 31, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it.
5. “How The Body Reacts To Viruses – HMX: Harvard Medical School.” HMX | Harvard Medical School. February 19, 2021. Accessed May 31, 2021. https://onlinelearning.hms.harvard.edu/hmx/immunity/.
6. Drexler, Madeline. What You Need to Know about Infectious Disease. Washington, D.C., WA: National Academies Press, 2010.
7. Yuki, Koichi, Miho Fujiogi, and Sophia Koutsogiannaki. “COVID-19 Pathophysiology: A Review.” Clinical Immunology 215 (2020): 108427. doi:10.1016/j.clim.2020.108427.
8. “Image Library.” Centers for Disease Control and Prevention. February 10, 2020. Accessed May 31, 2021. https://www.cdc.gov/media/subtopic/images.htm.
9. Yazdanpanah, Fereshteh, Michael R. Hamblin, and Nima Rezaei. “The Immune System and COVID-19: Friend or Foe?” Life Sciences 256 (2020): 117900. doi:10.1016/j.lfs.2020.117900.
10. Lee, Amanda J., and Ali A. Ashkar. “The Dual Nature of Type I and Type II Interferons.” Frontiers in Immunology 9 (2018). doi:10.3389/fimmu.2018.02061.
11. Scully, Eileen P., Jenna Haverfield, Rebecca L. Ursin, Cara Tannenbaum, and Sabra L. Klein. “Considering How Biological Sex Impacts Immune Responses and COVID-19 Outcomes.” Nature Reviews Immunology 20, no. 7 (2020): 442-47. doi:10.1038/s41577-020-0348-8.
12. Cornell, Brent. “Lung Tissue.” BioNinja. 2016. Accessed May 31, 2021. https://ib.bioninja.com.au/options/option-d-human-physiology/d6-transport-of-respiratory/lung-tissue.html.
13. Bussani, Rossana, Edoardo Schneider, Lorena Zentilin, Chiara Collesi, Hashim Ali, Luca Braga, Maria Concetta Volpe, Andrea Colliva, Fabrizio Zanconati, Giorgio Berlot, Furio Silvestri, Serena Zacchigna, and Mauro Giacca. “Persistence of Viral RNA, Pneumocyte Syncytia and Thrombosis Are Hallmarks of Advanced COVID-19 Pathology.” EBioMedicine 61 (2020): 103104. doi:10.1016/j.ebiom.2020.103104.
14. Wadman, Meredith. “How Does Coronavirus Kill? Clinicians Trace a Ferocious Rampage through the Body, from Brain to Toes.” Science, 2020. doi:10.1126/science.abc3208.
15. Barton, Lisa M., Eric J. Duval, Edana Stroberg, Subha Ghosh, and Sanjay Mukhopadhyay. “COVID-19 Autopsies, Oklahoma, USA.” American Journal of Clinical Pathology 153, no. 6 (2020): 725-33. doi:10.1093/ajcp/aqaa062.
16. Gaillard, Frank. “Normal Chest X-ray: Radiology Case.” Radiopaedia Blog RSS. Accessed May 31, 2021. https://radiopaedia.org/cases/normal-chest-x-ray?lang=us.Case courtesy of Assoc Prof Frank Gaillard, Radiopaedia.org, rID: 8304
17. Wang, Xingrui, Qinglin Che, Xiaoxiao Ji, Xinyi Meng, Lang Zhang, Rongrong Jia, Hairong Lyu, Weixian Bai, Lingjie Tan, and Yanjun Gao. “Correlation between Lung Infection Severity and Clinical Laboratory Indicators in Patients with COVID-19: A Cross-sectional Study Based on Machine Learning.” BMC Infectious Diseases 21, no. 1 (2021). doi:10.1186/s12879-021-05839-9.
18. Salehi, Sana, Aidin Abedi, Sudheer Balakrishnan, and Ali Gholamrezanezhad. “Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients.” American Journal of Roentgenology 215, no. 1 (2020): 87-93. doi:10.2214/ajr.20.23034.
19. Magro, Cynthia, J. Justin Mulvey, David Berlin, Gerard Nuovo, Steven Salvatore, Joanna Harp, Amelia Baxter-Stoltzfus, and Jeffrey Laurence. “Complement Associated Microvascular Injury and Thrombosis in the Pathogenesis of Severe COVID-19 Infection: A Report of Five Cases.” Translational Research 220 (2020): 1-13. doi:10.1016/j.trsl.2020.04.007.
20. Wichmann, Dominic, Jan-Peter Sperhake, Marc Lütgehetmann, Stefan Steurer, Carolin Edler, Axel Heinemann, Fabian Heinrich, Herbert Mushumba, Inga Kniep, Ann Sophie Schröder, Christoph Burdelski, Geraldine De Heer, Axel Nierhaus, Daniel Frings, Susanne Pfefferle, Heinrich Becker, Hanns Bredereke-Wiedling, Andreas De Weerth, Hans-Richard Paschen, Sara Sheikhzadeh-Eggers, Axel Stang, Stefan Schmiedel, Carsten Bokemeyer, Marylyn M. Addo, Martin Aepfelbacher, Klaus Püschel, and Stefan Kluge. “Autopsy Findings and Venous Thromboembolism in Patients With COVID-19.” Annals of Internal Medicine 173, no. 4 (2020): 268-77. doi:10.7326/m20-2003.
21. Hamblin, James. “Why Some People Get Sicker Than Others.” The Atlantic. August 19, 2020. Accessed May 31, 2021. https://www.theatlantic.com/health/archive/2020/04/coronavirus-immune-response/610228/.

