By Tara Allison, Biochemistry and Molecular Biology and Spanish ‘20
Author’s Note: I wrote this document as a UWP 102B assignment to evaluate the societal health care needs of Sacramento County, focusing on an upsetting mental health phenomenon, Adverse Childhood Events (ACEs). This review encompasses an in-depth analysis that illuminates the biological basis of ACEs and their connection to chronic health conditions in adulthood. This review further analyzes several Community Needs Assessments to ascertain that existing health care institutions do not, in fact, provide the proper focus or volume of mental health and ACE-related treatment needed for Sacramento County. The multidisciplinary nature of this paper connects scientific data that suggest a widespread health problem to an effective solution that UC Davis can adopt as a university. My on-campus organization R.I.V.E.R. (Recognizing Illnesses Very Early and Responding) is making progress towards development of this solution, a mobile pediatric ACE clinic.
1. Introduction
This review explores the potential benefits of developing a new mobile pediatric medical clinic that serves the northwest region of Sacramento County through Adverse Childhood Events (ACEs) related care. First, this review provides evidence of the community health needs in Sacramento County, discussed in three sections: what patients need, what currently exists for them, and what they need that is not currently offered. Second, this review examines the correlation between ACEs and future chronic health issues. And finally, this review proposes a solution based on successful existing mobile clinic models and associated limitations. For the studies included in this review, various criteria and characteristics were considered or excluded to achieve an accurate assessment of the ACE-related risk experienced by individuals in Sacramento and Palo Alto. Individuals not primarily living in these specified regions were excluded from these studies.
2. Community Health Needs In Sacramento County
2.a. What Patients Need
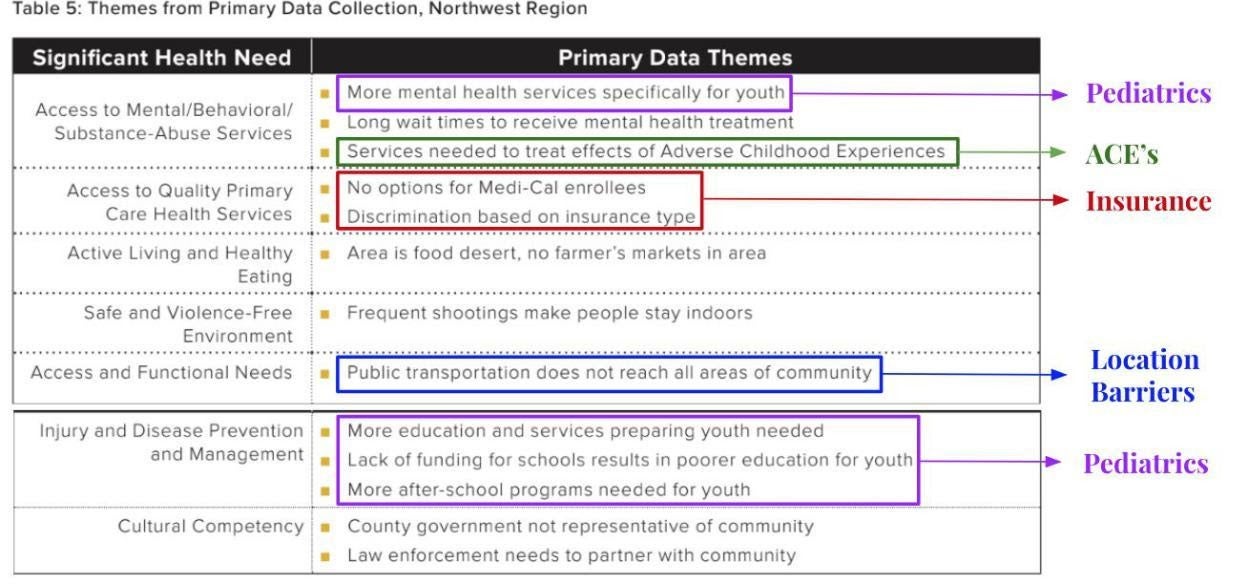
The northwest region of Sacramento specifically needs health care services for ACEs and primary care needs despite location and public transportation barriers and access to medical care regardless of insurance status. According to Table 5 of the 2019 Community Health Needs Assessment of Sacramento County, the northwest region of Sacramento lacks many types of health care services. Specifically, this area needs additional mental and behavioral health care services, access to quality primary care, and resources for active living and healthy eating. Additional factors contributing to an underwhelming health care sufficiency are lack of safe and violence-free environments, deficiency of functional mechanisms such as public transportation, reduced services for injury and disease prevention management, and shortage of overall cultural competency [1]. This table also explicitly highlights that youth populations need more mental health and ACE services. For the remainder of this piece, ACE-care can be considered a “mental, behavioral, and substance-abuse” service as indicated by the table.
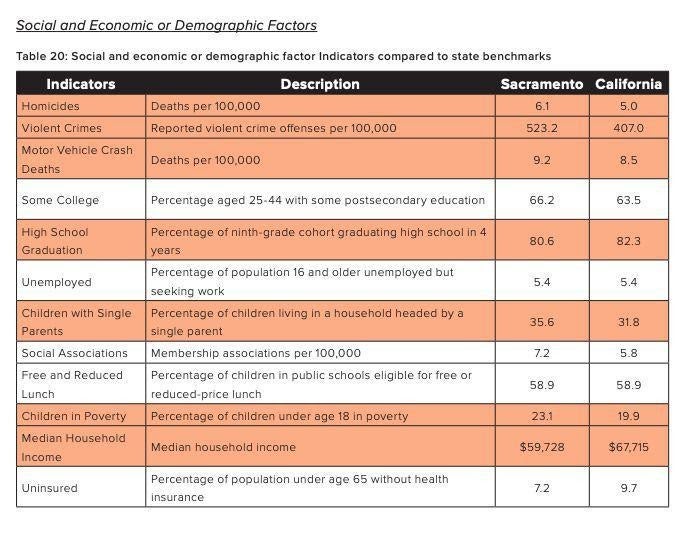
According to Table 20 of the 2019 Community Health Needs Assessment of Sacramento County, Sacramento County has higher rates of children in poverty and children with single parents than the California averages. The median household income is comparatively lower than the California average, and there is a higher rate of violent crimes and homicides in Sacramento than in California as well [1].
The 2016 Sacramento County Community Needs Assessment establishes that medically underserved areas are localized around several different zip codes in the Sacramento area. Within these regions, pediatric emergency department admission rates are 50 percent higher than county rates due to substance abuse, mental health issues, and asthma [2]. Among the zip codes listed, 95815 and 95841 appear again in the 2019 UCD Community Needs Health Assessment, indicating that from 2016 to 2019 the same regions were consistently in need of improved health care services. This suggests that existing health care organizations are not sufficiently serving these communities.
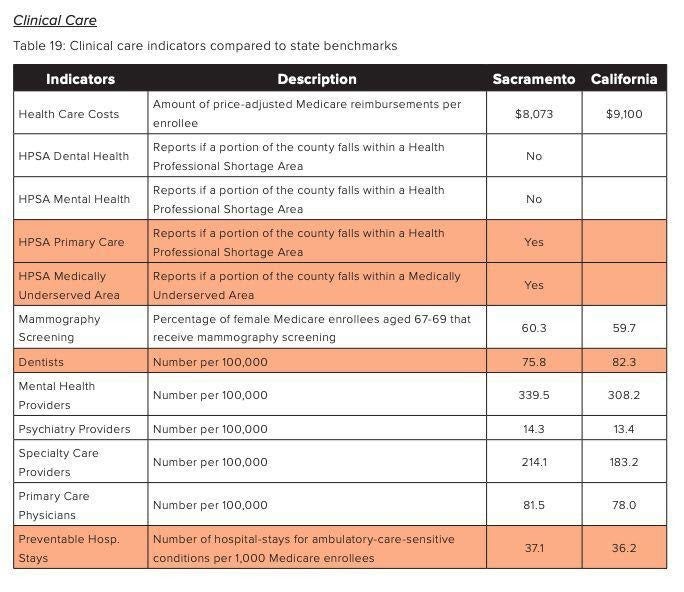
Table 19 of the 2019 UCD Community Needs Health Assessment indicates varying amounts of clinical care providers in Sacramento County compared to the California average. It reports that portions of Sacramento are in a health professional shortage area (HPSA) for primary care and are generally considered medically underserved. However, the number of mental health providers, psychiatry providers, and primary care physicians is above the ratio for California overall. This may suggest that the location of these providers is potentially inequitable, creating a disparity across various regions of Sacramento by unevenly distributing providers. This disparity is demonstrated by the northwest Sacramento region, which lacks adequate mental health and primary care provisions.
2.b. What Exists Currently
Interestingly, although Sacramento does not lack health care professionals for mental health services compared to the average California benchmark, quality of life indicates that Sacramento residents experience poorer mental and physical health than the average California resident. This suggests that distribution of such health care professionals is inadequate and that care is not being provided to enough regions. The 2019 UCD Community Needs Health Assessment demonstrates this very clearly with data describing existing health organizations. Sacramento County contains 281 existing health care organizations that provide a variety of services. Out of those 281 organizations, only 96 institutions, or 34 percent of them, provide access to mental, behavioral, or substance abuse services. Only 73 of 281 institutions, or 26 percent, provide access to quality primary care services. And only 81 of 281 institutions, or 29 percent, provide access to active living and healthy eating resources [1]. These institutions are distributed across all of Sacramento County, so the actual health care accessibility of specific communities varies. Thus, even though existing organizations are present in Sacramento to provide these services, they are not equitably distributed across the county or provided in a high enough volume to meet expansive geographical demands.
As indicated by Table 5 of the 2019 Community Health Needs Assessment of Sacramento County, additional factors such as quality of public transportation and safety of neighborhoods may also influence patient accessibility to health care [1]. Poorly developed public transportation and frequent crimes may create an environment that encourages potential patients to stay at home, even if they reside nearby a clinic or hospital. Thus, violent environments and reduced transportation combined with inequitably-distributed health care services equate to unmet health care demands. This data indicates that Sacramento may not be well-equipped to address its various medical needs across the county.
It might make sense to conclude that any region containing a higher concentration of health care institutions for mental health should have adequate health care coverage in this category. However, this is not a completely valid assumption. The 2019 UCD Community Needs Health Assessment reports surprising contrasts within particular zip codes. It demonstrates that some areas contain plenty of clinics that provide mental health, behavioral, and substance abuse services, yet these areas are still indicated as regions that are in significant need of those services. For example, within the zip code 95823, 8 of 21 health care institutions provide mental health services in that area. However, according to the 2019 UCD Community Needs Health Assessment, the zip code 95823 resides in a region that still lacks adequate mental health services [1]. Despite that almost half of the health care organizations within 95823 provide mental health services, there is still a demonstrated need for higher volume of service or improved focus on mental health care within community clinics. This data further demonstrates that existing health care organizations are not meeting patients’ needs and could suggest that existing clinics do not provide the correct types of services or adequate volume of care required for the community.
2.c. What is Lacking
There are three primary issues that the northwest region of Sacramento is experiencing. These include health care insurance denial from current providers, location and public transportation barriers to attain proper health care, and lack of primary care access and ACE-related care.
Despite the various health organizations available, the northwest portion of Sacramento still has three unaddressed significant health care needs. In order to address all three issues, a proposal to develop a new pediatric mobile clinic should be considered. To address insurance barriers, the new clinic will provide free services to all patients regardless of insurance status. To address location challenges, the clinic will function in a large mobile vehicle equipped for medical care providers. Not only can new patient locations be reached, but multiple regions can be served by this clinic. And finally, the mobile clinic will provide services to address primary care and ACE-related care needs.
3. Correlation Between Adverse Childhood Events and Chronic Mental, Behavioral, and Physical Health Issues
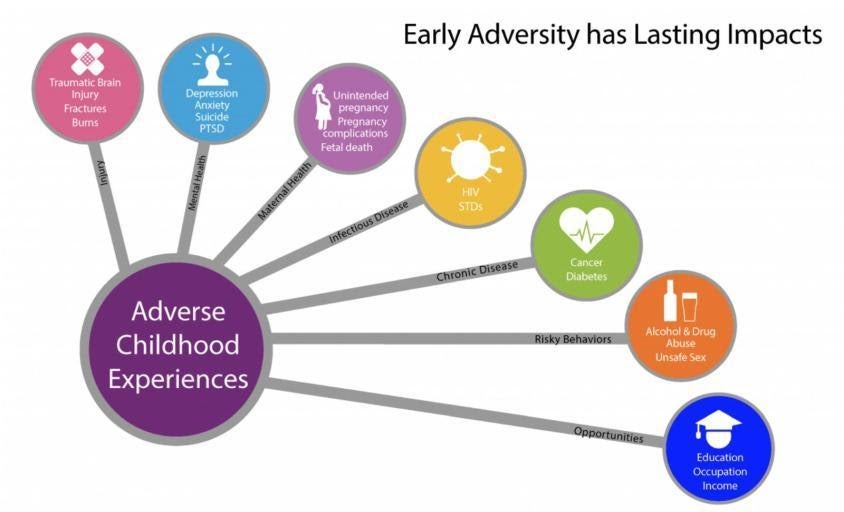
The Center for Disease Control and Prevention defines ACEs as mentally and emotionally traumatic experiences that affect adolescents before the age of 18. These traumatic experiences can exist in many forms. Some examples include growing up in a household with family members who abuse substances, have mental health problems, are incarcerated, or divorced. Such experiences can undermine children’s sense of stability and safety while simultaneously interfering with their ability to bond with family or friends [3]. Many years of seminal research in this topic demonstrate a myriad of connections between ACEs and chronic health conditions, unsafe health behaviors, and premature death. This discussion will utilize research older than two years ago that is foundational to these health correlations.
3.a. Chronic Health Issues
Chronic health conditions such as autoimmune disease, cancer, chronic obstructive pulmonary disease (COPD), frequent headaches, ischemic heart disease (IHD), prescription drug usage, and liver disease have been proven to result from individuals plagued by ACE-related trauma [4, 5, 6, 7, 8, 9]. Dube and colleagues demonstrate that traumatic events during adolescence correlate with an increased probability of autoimmune disease hospitalization during adulthood [4]. In addition, Ports et al. establish a strong correlation between ACEs and exposure to modifiable cancer risks such as alcohol, chronic inflammation, obesity, UV radiation, and environmental carcinogens. Additionally, this study suggests that addressing ACEs may induce early cancer prevention [5]. Cunningham and colleagues study the correlation between COPD and ACEs such as verbal and sexual abuse, parental separation or divorce, observation of substance-abusing family members, and domestic violence. Their results indicated a higher chance of developing COPD if one or more of these ACEs were experienced in women specifically [6]. Another study by Anda and colleagues studied the relationship between the prevalence of headaches and migraines and the presence of ACEs. The results indicated that, in adulthood, there was a higher frequency of headaches or migraines if the subject had a higher ACE risk score. Subjects with lower or nonexistent ACE risk scores experienced far fewer headaches [7]. Additionally, a study completed by Dong and colleagues illuminates the connection between several types of ACEs and development of IHD. Their results demonstrate a 1.3 to 1.7 fold increase in the chance of developing IHD for patients experiencing more ACEs in comparison to those with a low ACE risk score [8]. In a different study, Dong and colleagues examine correlation of ACEs to risky behaviors that manifest later in life as liver disease. ACEs increased the likelihood of liver disease development by 1.2 to 1.6 times [9]. Beyond chronic health issues, ACEs have been shown to be related to other problems in adulthood such as unsafe health behaviors.
3.b. Unsafe Health Behaviors
Unsafe health behaviors such as alcohol abuse, drug use, obesity, sexual risk behavior, and smoking are health outcomes of ACEs as well [10, 11, 12, 13, 14]. Strine et al. establishes direct correlations between alcohol abuse and ACE-related experiences such as sexual abuse, childhood neglect and emotional abuse, family drug abuse or mental illnesses, and parental divorce. They claim that psychological distress associated with ACEs results in alcohol abuse later in life [10]. Furthermore, Anda and colleagues discovered a 40 percent increase in prescription drug usage in patients with non-zero ACE scores and a positive correlation between a higher ACE risk score and prescriptions across all age groups (18-44, 45-64, and 65-89 years of age) [11]. In another study, Williamson and colleagues identified a correlation between physical and verbal abuse and increased body weight and obesity measurements. Participants that experienced “being hit” were 4.0 kg heavier on average than participants that did not report physical abuse [12]. Additionally, Hillis et al. evaluated the connection between sexual risk behavior and ACE events and discovered a positive correlation between the two as well [13]. Strine and colleagues, in a different study, observed increased risk of smoking habits in women when ACE risk scores are present as well [14]. ACEs have been shown to relate to reduced lifespans as well.
3.c. Premature Death
ACEs correlate with suicide and depression in adulthood, leading to premature death in adulthood [15, 16]. According to Dube and colleagues, suicide rates increased two to five fold in adulthood due to connections regarding ACEs. Factors such as alcoholism and illicit drug use had close ties to the presence of ACEs and path to suicide attempt [15]. Additionally, Chapman et al. established a connection between a higher number of ACE-related events and a greater chance of developing a depressive disorder. The study also suggests that early recognition of childhood trauma may prevent future depression diagnosis [16]. This extensive, yet not exhaustive, collection of studies indicates that ACEs have a very real impact on pediatric mental health and adult health status later in life. In order to address the lack of mental health provision in Sacramento, the proposal to develop a new pediatric mobile clinic specializing in ACE-care and primary care services should be considered.
4. Proposed Solution and Limitations
The northwest region of Sacramento has three primary concerns: health care insurance denial from current providers, location and public transportation barriers to attain proper health care, and lack of primary care access and ACE-related care. In order to address these issues, this paper proposes the implementation of a new mobile medical pediatric clinic. The clinic will provide ACE-related care and primary care services for chronic and acute illnesses. It will mitigate health care insurance barriers by serving uninsured and partially insured residents of Sacramento County as well. Furthermore, the clinic will serve patients in a 26-foot vehicle equipped with two medical examination rooms and ample supplies. In this way, residents can access medical care despite any location or public transportation challenges. As a vehicular clinic, mobility ensures access to multiple communities in Sacramento.
The primary barriers to implementing this mobile clinic include shortage of staffing availability along with annual financial demands. These are not issues unique to a mobile or pediatric ACE-care clinic, so our proposal can model existing clinics to realistically overcome these barriers. First, UC Davis student-run clinics are excellent models to consider. Financially, a volunteer-based operations system will ensure low-cost annual expenditures. Furthermore, grant writing, fundraising, and donor support are effective funding methods these successful clinics utilize as well. Staffing availability can be mitigated by way of a reduced, yet consistent, weekend operations schedule. As physicians may not be available during weekdays due to employment commitments, weekends are an ideal time to volunteer.
We can observe many similarities between this mobile, ACE-care, pediatric clinic proposal and other vehicular clinic models. Existing mobile medical clinics provide similar services in other cities and provide excellent examples to base this proposal on. One especially successful case is the Stanford Teen Van, a mobile medical clinic that primarily serves youth in the Bay Area. The table below from the 2019 Stanford Community Health Needs Assessment indicates that this clinic provides ACE-related care in the form of mental health services in addition to primary care. Furthermore, this establishment has successfully provided improved access for 2,892 individuals that otherwise would experience location-based barriers [17].
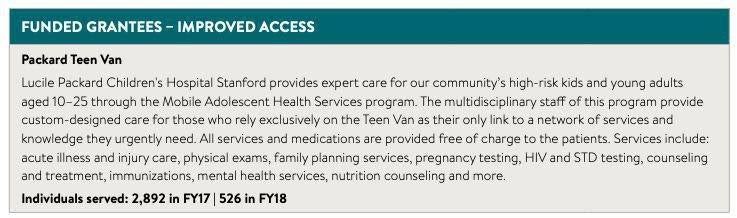
The Stanford Teen Van also provides its services and medications for free, thus eliminating any insurance-based discrimination. This model is an excellent comparison to study because this clinic provides identical services to a similarly underserved population in the Bay Area. The Stanford Teen Van, alongside the UC Davis student-run clinics, are phenomenal infrastructures to learn from by way of mobility, service provision, and volunteerism. By analyzing successful practices, this proposal overcomes limitations and provides effective solutions based on existing infrastructures, resulting in a refined and well-rounded project concept.
5. Conclusion
This review discussed the potential benefits of developing a new mobile pediatric medical clinic that would serve the northwest region of Sacramento County. First, this review demonstrated extensive evidence of the community health needs in Sacramento. Second, this review examined the correlation between ACEs and future chronic health issues. Finally, this review discussed a proposed solution following successful existing mobile clinic models and associated limitations. When considering the data holistically, it is clear that a new pediatric mobile clinic would significantly benefit deserving patients in Sacramento. Furthermore, despite the fact that this mobile clinic proposal is built on well-established practices and successful existing infrastructure, this specific combination of ideas has not yet been implemented in Sacramento. While maintaining its merit and validity, this innovative project challenges the existing medical culture of Sacramento by introducing ACE awareness and the expansive versatility of a mobile clinic vehicle.
References
- Ainsworth D, Diaz H, Schmidtlein M, Van T, 2019 Community Health Needs Assessment. 2019 CHNA of Sacramento County 2019. 2019; 1-116.
- Wagner J, Rosenbaum A, Schmidtlein M, Underwood S. Sacramento County Community Health Needs Assessment. Sacramento County CHNA. 2016; 1-40.
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine. 1998; Vol 14, Issue 4, 245-258.
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune disease. Psychol Med. 2009; 71:243–250.
- Ports KA, Holman DM, Guinn A, Pampati S, Dyer K, Merrick MT, Buchanan N, & Metzler M. Association between Adverse Childhood Experiences and Leading Risk Factors for Cancer in Adulthood. Journal of Pediatric Nursing. 2019; 44, 81-96.
- Cunningham TJ, Ford ES, Croft JB, Merrick MT, Rolle IV, Giles WH. Sex-specific relationships between adverse childhood experiences and chronic obstructive pulmonary disease in five states. 2014; 9:1033-42.
- Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache. 2010; 50(9):1473-81.
- Dong M, Giles WH, Felitti VJ, Dube, SR, Williams JE, Chapman DP, Anda RF. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004; 110:1761–1766.
- Dong M, Anda RF, Dube SR, Felitti VJ, Giles WH. Adverse childhood experiences and self-reported liver disease: new insights into a causal pathway. Arch Intern Med. 2003; 163:1949–1956.
- Strine TW, Dube SR, Edwards VJ, Prehn AW, Rasmussen S, Wagenfeld M, Dhingra S, Croft JB. Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. Am J Health Behav. 2012; 36(3):408-23.
- Anda RF, Brown DW, Felitti VJ, Dube SR, Giles WH. Adverse childhood experiences and prescription drug use in a cohort study of adult HMO patients. BMC Public Health. 2008; 4; 8:198.
- Williamson DF, Thompson, TJ, Anda, RF, Dietz WH, Felitti VJ. Body weight, obesity, and self-reported abuse in childhood. International Journal of Obesity. 2002; 26:1075–1082.
- Hillis SD, Anda RF, Felitti VJ, Marchbanks PA. Adverse childhood experiences and sexual risk behaviors in women: a retrospective cohort study. Fam Plann Perspect. 2001; 33:206–211.
- Strine TW, Edwards VK, Dube SR, Wagenfeld M, Dhingra S, Prehn AW, Rasmussen S, Mcknight-Eily L, Croft JB. The mediating sex-specific effect of psychological distress on the relationship between adverse childhood experiences and current smoking among adults. Subst Abuse Treat Prev Policy. 2012; 7:30.
- Dube SR, Anda RF, Felitti VJ, Chapman D, Williamson DF, Giles WH. Childhood abuse, household dysfunction and the risk of attempted suicide throughout thelife span: Findings from Adverse Childhood Experiences Study. JAMA. 2001; 286:3089–3096.
- Chapman DP, Anda RF, Felitti VJ, Dube SR, Edwards VJ, Whitfield CL. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004; 82:217–225.
- Espino M, Stelle J. 2019 Community Health Needs Assessment. 2019 Stanford Community Health Needs Assessment. 2019; 1-52.

