By Reshma Kolala, Biochemistry & Molecular Biology ‘22
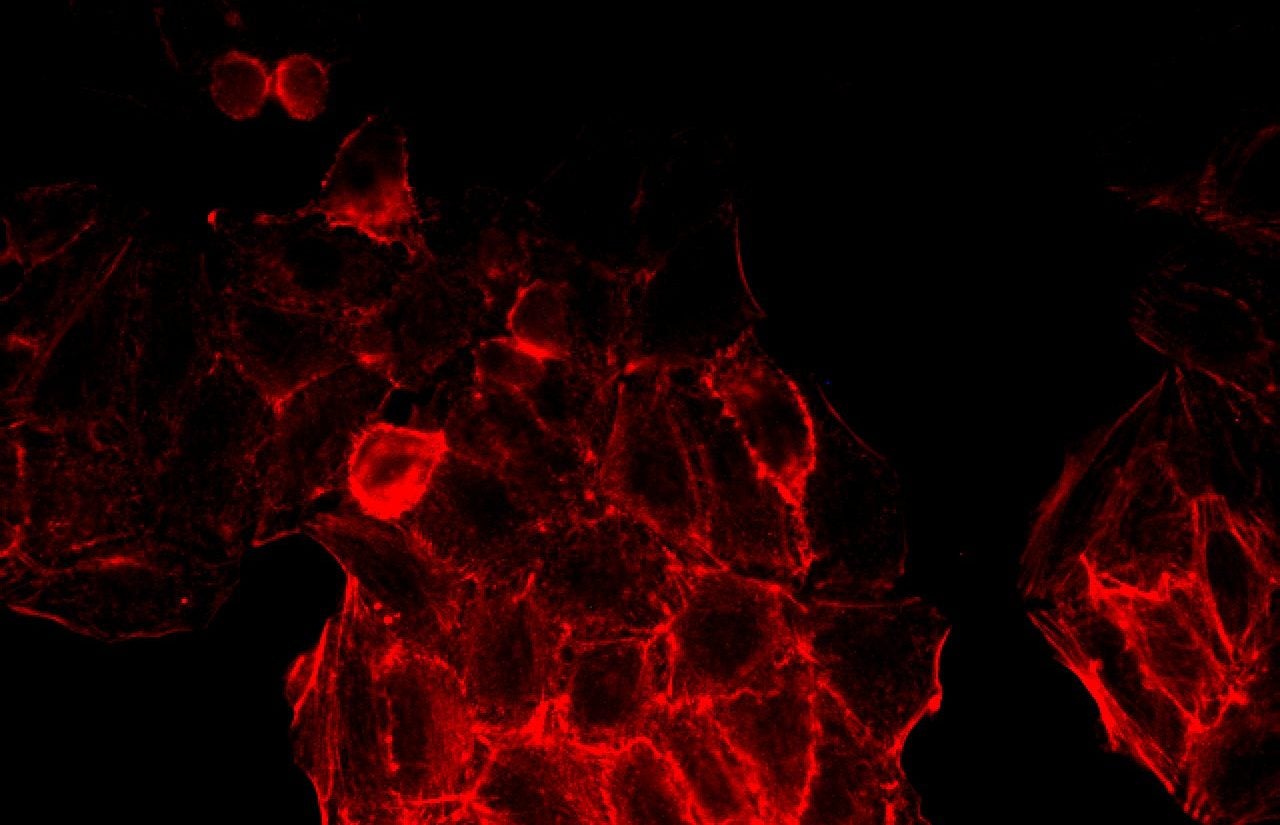
Residing in the pancreas are clusters of specialized cells, namely alpha, beta (), and delta cells. cells, more specifically, are insulin-secreting cells that are instrumental in the body’s glucose regulation mechanism. An elevation of the extracellular glucose concentrations allows glucose to enter cells via GLUT2 transporters, where it is subsequently metabolized. The resultant increase in ATP catalyzes the opening of voltage-gated Ca2+ channels, triggering the depolarization of the plasma membrane which in turn stimulates insulin release by cells (1). In individuals with Type 1 Diabetes (T1D), however, pancreatic islet beta cells are damaged by pro-inflammatory cytokines that are released by the body’s own immune cells. The loss of functional beta cell mass induces a dangerous dysregulation of glucose levels, resulting in hyperglycemia along with other harmful side effects. The absence of a regulatory factor in the bloodstream forces those with T1D to take insulin intravenously to remedy the consequences.
A new study led by Dr. Ercument Dirice, a Harvard Medical School (HMS) instructor and research associate at the Joslin Diabetes Center. has suggested that an increase in cell mass early in life diminishes the autoreactive behavior of immune cells towards cells, therefore halting the development of T1D (2). In a typical T1D model, the secretion of antigens from cells induces a response from the body’s immune cells. These immune cells bind to the epitopes (the recognizable portion of an antigen) that are displayed on the surface of professional antigen presenting cells (APC’s) which are littered throughout the pancreatic islets (3). This binding action induces a destructive autoimmune response to antigens secreted by cells, resulting in loss of functional beta-cell mass. It was found however that by increasing cell mass at an early age where the organs of the immune system are still developing, the immune cells stopped attacking cells.
The novel approach presented by Dirice et al. departs from the traditional method of targeting various other components involved in the destructive autoimmune response, namely APC’s or the pro-inflammatory cytokines associated with T1D progression. This method instead focuses on the source of the autoimmune marked “pathogenic” antigens, the cells themselves.
The studies were completed using two models of female non-obese diabetic (NOD) mice. One was a genetically engineered model of female mice (NOD-LIRKO) that showed increased cell growth soon after birth while the second model was done using a live mouse that was injected at an early age with an agent known to increase cell proliferation. While maintaining more than 99.5% isogenicity (4), it was found that the mice with increased cell mass had a significantly lower predisposition to develop diabetes when compared against the NOD control mice, which developed severe diabetes between 20-35 weeks of age. The study also observed the interaction between the modified cells and immune cells by monitoring the concentration of these immune cells in the spleen. In doing this, researchers were able to conclude which mice had a greater risk of developing T1D based on if mice had an abnormal increase in the concentration of these cells.
At first glance, this method appears counterintuitive as an increase in cell mass may lead one to naively assume that this would result in increased autoantigen production. This precise hypothesis illustrates the beauty of this approach. Although the specific details of this mechanism have yet to be made clear, it is believed that the rapid turnover of cells “confuses” the autoimmune reaction. The proliferated cells present unusual autoantibodies that are not observed in typical T1D progression. Dr. Rohit Kulkarni, a fellow HMS professor and researcher at Joslin noted that there is thought to be some alteration in the new cells where the autoantigens typically produced are reduced or dilated (2). As a result of the slow presentation of antigens, there is a lower proportion of autoreactive immune cells. This essentially results in a “reshapen immune profile that specifically protects cells from being targeted.” Some degree of autoimmunity would continue to exist in the body, so further immunosuppressive treatment would be required.
Early cell proliferation has been previously speculated to have a protective effect in those with reduced functional cell mass as in a Type 1 Diabetes model. Once this preventative quality is better understood, applications of this research may be further explored. Despite still being in the beginning stages, this novel approach holds tremendous potential for application to T1D if this method is able to be translated to a human model. The massive prevalence of a T1D diagnosis is illustrated by 2014 census data that states that T1D affects roughly 4.7% of the world’s adult population. Although extensive research continues to be done on several aspects of the disease, the introduction of new data by Dirice et al. may push us a small step closer to solving one of the body’s greatest metabolic mysteries.
References
- Komatsu, M., Takei, M., Ishii, H., & Sato, Y. (2013, November 27). Glucose-stimulated insulin secretion: A newer perspective. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4020243/
- Yoon, J., & Jun, H. (2005). Autoimmune destruction of pancreatic beta cells. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16280652
- Pushing early beta-cell proliferation can halt autoimmune attack in type 1 diabetes model. (2019, May 06). Retrieved from https://www.sciencedaily.com/releases/2019/05/190506124102.htm
- Burrack, A. L., Martinov, T., & Fife, B. T. (2017, December 05). T Cell-Mediated Beta Cell Destruction: Autoimmunity and Alloimmunity in the Context of Type 1 Diabetes. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5723426/
- Dirice, E., Kahraman, S., Jesus, D. F., Ouaamari, A. E., Basile, G., Baker, R. L., . . . Kulkarni, R. N. (2019, May 06). Increased β-cell proliferation before immune cell invasion prevents progression of type 1 diabetes. Retrieved from https://www.nature.com/articles/s42255-019-0061-8?_ga=2.76180373.1669397493.1557550910-1092251988.1557550910