By David Ivanov, Biochemistry and Molecular Biology, 2015
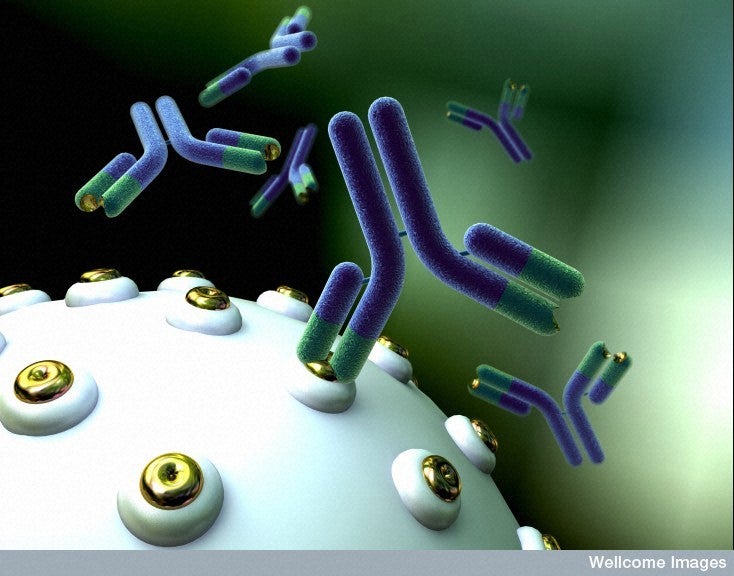
Sjogren’s syndrome, like other autoimmune diseases, can be difficult to diagnose definitively, and often relies on a handful of signs and symptoms that can vary substantially from case to case. The only signs considered markers for Sjogren’s are anti-SSA and anti-SSB antibodies, and while anti-SSB is more specific, elevated levels of anti-SSB are actually less common in patients with Sjogren’s syndrome than anti-SSA, leading to some ambiguity in diagnosis.
A seventeen year old female patient presented with a large, soft, sublingual cyst on the left side of the floor of her mouth. While she reported no pain, the cyst was first spotted about a year earlier, and had been growing steadily. Visible swelling was observed on the left side of her face under her jaw line. Surgery was performed to remove the cyst, and an adjacent salivary gland was removed as well. The otorhinolaryngologist took a tissue sample, and histology confirmed a benign growth. The surgeon ordered a blood panel to evaluate antibody levels that might indicate an autoimmune disease. The patient’s serum was negative for rheumatoid factor, anti-SSB antibodies, and anti-nuclear antibodies. However, she was positive for anti-SSA antibodies, with a level of 50 U/ml. Bacterial cultures were negative for oral infection, and an X-ray was negative for sarcoidosis. Patient was discharged after surgery with no medications indicated, as she was not experiencing any other symptoms.
At age twenty, the patient again noticed a sublingual cyst on the floor of her mouth, this time on her right side. Upon inspection, the otorhinolaryngologist confirmed the presence of a lymphangioma. Two months later, it had grown and caused the adjacent sublingual salivary gland to rupture, resulting in a ranula at the floor of her mouth. The patient sought treatment, and the otorhinolaryngologist ordered an MRI to examine the ranula. The lymphangioma was found to be growing towards another salivary gland, presumably causing the sialadenitis observed in that gland. The ranula and the ruptured sublingual salivary gland were then surgically excised. Histology again ruled out malignancy, but suggested Sjogren’s syndrome or another autoimmune disease.
The ENT surgeon referred the patient to a rheumatologist, who performed a blood panel to rule out other autoimmune disorders. The patient was again negative for rheumatoid factor and her erythrocyte sedimentation rate was normal. However, her IgG subclass 4 levels were 253 mg/ml, well beyond the normal range of 0-150 mg/ml.
The rheumatologist also tested for other signs and symptoms of Sjogren’s. The patient was negative for dry skin, dry mouth, joint pain, circulation or perfusion issues, and general fatigue. Family history was mostly negative for any signs or symptoms of Sjogren’s aside from the patient’s mother having dry eyes. The mother reported no other symptoms and was not tested for Sjogren’s syndrome. No other additional abnormalities were observed.
The patient was sent home but placed under observation with biannual checkups for three years after the second surgical removal of the cyst, and annual checkups indefinitely after that. Three months later, she complained of mild to moderate skin dryness, and was prescribed Lac-Hydrin 12% lotion and urea 40% lotion. An optometrist noticed mildly dry eyes, but no treatment was suggested. The patient currently lives otherwise symptom-free and has not had any recurrence of abnormal growths in her mouth.
Discussion
Sjogren’s syndrome (SS), named after the Swedish ophthalmologist who first reported on the condition, is a relatively common autoimmune disease, affecting up to 2 million people in the United States. In patients with SS, the immune system attacks the salivary and lacrimal glands, causing dry mouth and dry eyes, respectively. There is no known cause of Sjogren’s syndrome, and no preventative treatment is known. However, genetic factors and environmental factors are suspected of playing a role in the development of the syndrome. There is some indication of high gluten sensitivity in patients with Sjogren’s syndrome, which can be related to the inflammation that gluten is known to potentially cause. Viral infections may also potentially increase the likelihood of SS through molecular mimicry that triggers autoimmunity.
Common symptoms of SS are dry mouth, dry eyes, dry skin, and less often, general fatigue, rashes, and joint pain. The most typical symptoms are dry eyes and dry mouth, which range in severity. Some patients have mild discomfort, while others can experience blurry vision and chronic eye irritation, and patients with dry mouth can have difficulty swallowing or eating dry foods and an increased likelihood of tooth decay. Most patients with the disorder have mild to moderate symptoms, but in rare cases, SS can cause organ failure. Patients are also more susceptible to non-Hodgkin’s lymphoma, a cancer of the white blood cells. About 5% of patients with Sjogren’s syndrome will have a malignant growth, but overall, the mortality rates of patients with SS are very similar to the normal population. While the symptoms are usually well managed and patients can live comfortably, patients who get pregnant have an increased risk of their elevated antibodies crossing the placenta and causing neonatal lupus erythematosus with a congenital heart block that requires a pacemaker.
While treatments of the condition are currently not known, drugs that help manage symptoms can be prescribed to patients with moderate to severe symptoms. Artificial tears or eye lubricants can be used to alleviate dry eyes, and cyclosporine can reduce loss of eye moisture by reducing ocular inflammation that can inhibit secretion of tears. A punctal plug can also be inserted to slow the rate of tear drainage and allow tears to continue lubricating the eye for a longer time. Several OTC mouthwashes are available to reduce oral dryness, and cevimeline can be used to stimulate salivation. Hydroxychloroquine can be used to treat joint pain and rashes on a symptomatic basis. More severe systemic symptoms, especially of the internal organs, can be treated with corticosteroids or other immunosuppressive drugs, but must be used with caution due to increased risk of infections. Patients, particularly those with dry mouth, must be regularly monitored for tooth decay, as dental caries are quite common and can progress to severe decay if left untreated.
Like other autoimmune disorders, Sjogren’s syndrome is difficult to diagnose definitively, and relies on antibody levels, physical signs, and patient symptoms. The oral cavity in particular must be examined for any growths associated with salivary gland occlusion or blockage. Elevated levels of anti-nuclear antibodies can indicate SS, and are present in about 70% of patients. Rheumatoid factor is also common in SS patients (60-70%) but can be indicative of other inflammatory conditions such as rheumatoid arthritis. Elevated levels of IgG subclass 4 are also commonly found in SS patients but are not specific. The antibodies that are considered actual markers for SS are anti-SSA and anti-SSB antibodies. While elevated anti-SSA antibodies are more common than anti-SSB antibodies in SS patients (about 70% vs 40%), the latter is a more specific marker for SS, while the former can also indicate systemic lupus erythematosus.
Since Sjogren’s syndrome can be secondary to systemic lupus erythematosus or rheumatoid arthritis, it is essential for healthcare providers to rule out these potentially more severe diseases. Diagnosing them, especially systemic lupus erythematosus, can be difficult since there are not any exact, definitive markers or tests available. A rheumatoid factor assay is essential on any blood panel, since that is an indicator of rheumatoid arthritis, and an x-ray to rule out sarcoidosis in the lungs is recommended to avoid missing an underlying cause of rheumatoid arthritis that may look like simply SS on a blood test. The SS markers anti-SSA and anti-SSB must be included on the blood panel as well, but since anti-SSA is also indicative of lupus, caution should be used in diagnosing a patient with SS until other antibody levels are assessed and a thorough physical examination is performed.
References
[SSF] Diagnosis. Sjogren’s Syndrome Foundation. 2014. Available from:https://www.sjogrens.org/home/about-sjogrens-syndrome/diagnosis (Acessed May 2015)
[SSF] Symptoms. Sjogren’s Syndrome Foundation. 2014. Available from:https://www.sjogrens.org/home/about-sjogrens-syndrome/symptoms (Acessed May 2015)
Wise, B. Sjogren’s Syndrome. American College of Rheumatology. 2012. Available from:
https://www.rheumatology.org/Practice/Clinical/Patients/Diseases_And_Conditions/Sj%C3%B6gren_s_syndrome/ (Accessed May 2015)
Tzioufas, A. Update on Sjögren’s syndrome autoimmune epithelitis: from classification to increased neoplasias. Clinical Rheumatology. December 2007. Volume 21, Issue 6
Manthrope, R. Late neonatal lupus erythematosus onset in a child born of a mother with primary Sjögren’s syndrome. Annals of Rheumatic Diseases. November 2004. 63(11):1496-7