A review on retinal migraines: the structural changes that occur on the retinal vasculature
Abstract
The mysteries of migraines, let alone retinal migraines—a rare disorder—have puzzled many researchers. Retinal migraines are characterized by episodes of transient monocular visual impairment combined with typical migraine symptoms. Retinal migraines were only officially introduced as a term in 1988 but terms such as “ocular migraine”, “ophthalmic migraine”, or “anterior pathway migraine” have been used interchangeably. This literature review examines the underlying characteristics of retinal migraines concerning their retinal vasculature and retinal nerve fibers. Many of the studies compared saw significant differences between migraine with aura (migraine with aura) and migraine without aura (migraine without aura) in the vascular density of the retinal vasculature [8]. Furthermore, those experiencing retinal migraines had a significantly thinner retinal nerve fiber layer than healthy controls [9]. Some studies utilized MRI to examine the retinal nerve fibers of patients and explored how white matter could play a role in retinal migraines. Additionally, evidence suggests the need for blood thinners or clot neutralizers that use invasive strategies to limit the decrease in retinal vascular density. Minimizing the apparent decrease in the retinal nerve fibers and retinal vascular density may lead to less monocular visual impairment during retinal migraines.
Introduction
Migraines have had extensive studies performed on them for decades, but retinal migraines are a rare disorder with an inconsistent name and diagnostic criteria. Initially, Polish ophthalmologist Xavier Galezowski 1882 referred to these types of migraines as “ophthalmic megrims'', which later branched off into unofficial terms such as “ophthalmic migraine”, “ocular migraine”, and “anterior pathway migraine” [1]. Not until 1988, that the term “Retinal Migraine” became an internationally agreed-upon definition when classified by the International Classification of Headache Disorders (ICHD) [1].
ICHD recognizes retinal migraines as a series of transient monocular visual impairment attacks that become coupled with a migraine headache [2]. Retinal migraines can still be diagnosed regardless of aura as they may occur even in the absence of an aura. A typical migraine aura is a temporary and fully reversible sensory disturbance that occurs before a migraine headache [3]. These disturbances include numbness or temporary loss of sensation, muscle weakness, impaired or temporary loss of vision, or difficulty in comprehending speech [4]. Aura occurs in about 30% of patients with migraine, and in 90% of those with migraines and aura, a visual disturbance is the most prominent and commonly exhibited type of aura [4]. And in those diagnosed with retinal migraine, the visual aura only affects one eye (monocular). Since the frequency and intensity of these visual disturbances vary between individuals, most studies find relevance in comparing the physiology of the retina, not only of healthy controls to retinal migraine patients but also to retinal migraine patients with or without aura.
Chong et al., Grosberg et al., Maher et al., and Lai et al. insist that a patient be diagnosed with retinal migraines if they present with the following symptoms: transient visual impairment in one eye, such as scintillations (seeing twinkling lights), scotoma (areas of decreased or lost vision), or temporary blindness [1-4]. The underlying cause of retinal migraines remains largely unknown and might be due to a variety of factors. Most notable factors are genetic risk factors that lead to decreased blood exchange in the retina from the narrowing of blood vessels or, more severe, retinal angiopathy (bursting of red blood cells) [1-3]. Furthermore, reviews performed by Chong et al., Grosberg et al., and Maher et al. which examined a wider range of individuals in terms of sex and age, revealed that retinal migraines disproportionately impact female patients at a significantly higher rate than male patients, with the most prevalent age group being at a mean of 24.7 years [1-3].
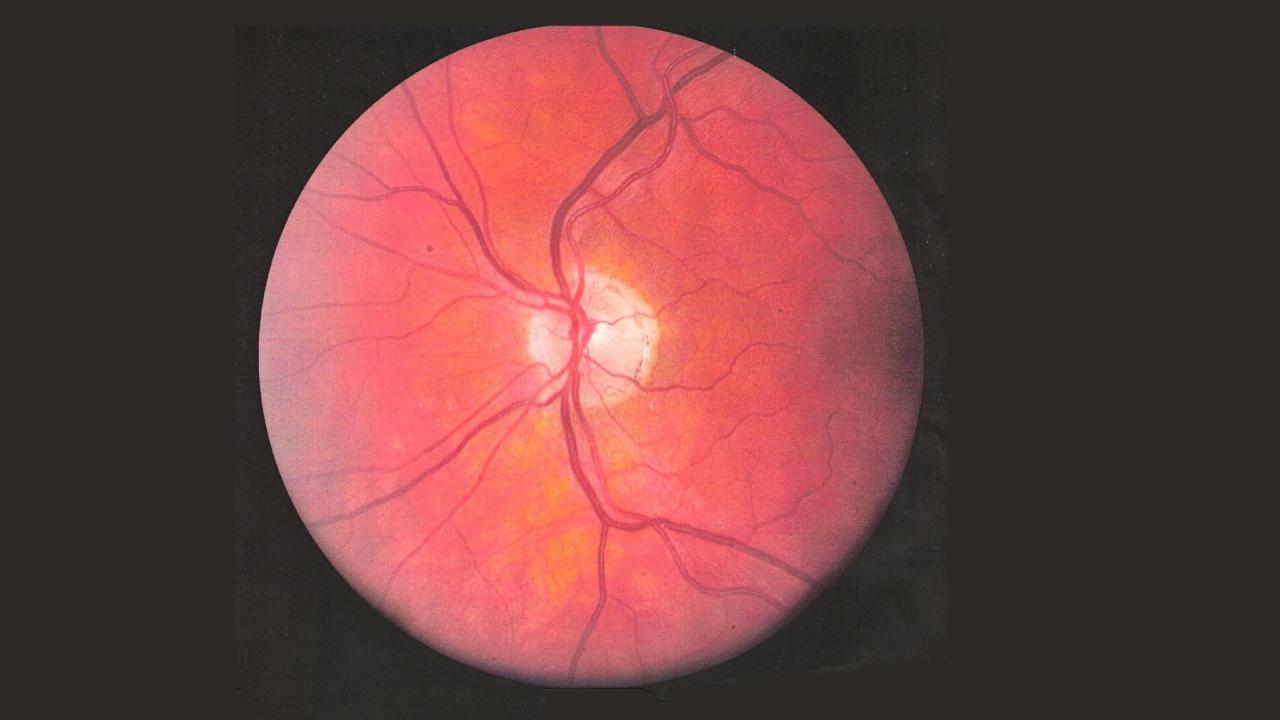
While the cause of retinal migraines is still unknown, two primary contributors have begun to emerge from the literature. Researchers currently believe that depression of electrical activity in the neuron might be causing the thinning seen in the retinal nerve fiber layer (RNFL). The underlying reason for this apparent depression is due to the slow-diffusing wave of depolarization that halts the function and speed of neuronal firing, leading to a diminished response in the RNFL [4]. The RNFL consists of axons from retinal ganglion cells. These axons converge at the optic disc and then pass through the optic canal, ultimately forming the optic nerve. The RNFL serves as the primary pathway for visual information to be collected by the photoreceptors (specifically, the rods and cones) of the retinal ganglion cells. From there, the visual signals travel along the axons of the RNFL ganglia to reach the brain [5]. The thinning of this layer reflects the loss of axons and signs and symptoms of visual impairment [5]. In Abdelghaffar et al. they observed that retinal migraines exhibit a transient and episodic nature, occurring in bursts. Over time, this pattern of occurrence may gradually alter the structure of both the brain and the retina negatively which leads to an abnormal change in the structure and formation of ganglion cells within the retina, potentially leading to their ultimate death [6]. Lin et al. also speculate that the death of the retinal ganglion cells, causing the reduction in the RNFL may be connected to vasoconstriction of the central retinal artery which causes changes in the blood supply and thus hypoxic injury to the optic nerve. Irregularities of the optic nerve in the retina is of particular interest since it is seen as a main contributor to the pathology of retinal migraines. Its apparent interconnectedness to other blood vessels (among of which is the central retinal artery) and neuronal layers coupled with the fact that it leads to the brain areas associated with vision is of prime interest to researchers.
Researchers were able to draw these conclusions by using a special imaging technique called Optical Coherence Tomography Angiography (OCTA) which uses lasers to visualize the different parts of the eye and monitor the movement of blood cells in the vasculature of the retina [1,4]. It also examines signals transmitted by retinal ganglion cells.
Structural changes in the Thickness of Retinal Nerve Fiber Layers
In the observational and cross-sectional study conducted by Reggio et al., OCTA imaging was utilized to closely examine the precise thickness of the RNFL layer in 77 patients who had migraines both with and without aura [9]. These patients were surveyed against healthy controls exhibiting no history of migraines [9]. OCTA imaging found that patients experiencing episodic or chronic migraines with aura had a thinner RNFL compared to closely related healthy controls [9]. After looking for connections between vascular abnormalities, including ischemia (reduction in blood flow) and vasospasm, and the RNFL there was no apparent statistical difference between the vasculature of the retina between migraine patients without aura versus migraine patients with aura [9]. However the researchers do propose that several reports have found links between vascular abnormalities and optic nerve damage.
In a separate study conducted by Y. Chang et al., female migraine patients, on average, had a thinner RNFL (97 ± 1.8 μm) than healthy control patients (104 ± 2.1 μm) [11]. This finding was proportional with an enlarged FAZ (foveal avascular zone) in female patients indicating the presence of microangiopathy which negatively impacts the retina’s ability to perceive color [11]. Additionally, in Yurtoğulları et al.’s study, women with retinal migraines (mean age of 32.5 ± 7.7 years) showed significantly thinner macular RNFL thickness, located in the middle of the retina, in both the migraine with aura and migraine without aura groups when compared to female healthy controls [13]. The thinner macular RNFL is likely due to angiopathy to the choroid (the vascular layer of the eye separating adjacent to the retina). This conclusion is reasonable to assume since blockage of choroidal blood flow is seen to cause ganglion cell death and the macula has a high concentration of ganglion cells [13].
Researchers in Reggio et al.’s study quantified the severity of migraines and saw an inverse relationship between RNFL thickness and headache intensity, that is, as the intensity of headaches increased, the thickness of the RNFL decreased [9]. More consistently, an inverse correlation also exists between the number of days of headache per month and RNFL thickness. This finding suggests that the number of days and severity of headaches plays a role in visual impairment in the retina. Yurtoğulları et al.’s study supports the notion that the initial decrease in ganglion cells appears to result from reduced blood flow to the retina, and recurrent retinal migraines over several years further contribute to a significant reduction in the RNFL [13].
Comparison of Retinal Nerve Fiber Layers in Migraine Patients With and Without Aura
In comparing the RNFL in patients with and without aura in Y. Chang et al’s cross-sectional study, there was no significant difference seen however in Ao R. et al.’s cross-sectional study, a significantly thinner RNFL in migraine with aura patients was seen compared to migraine without aura groups but to a lesser degree than that of those with aura patients to healthy control patients [12]. Furthermore, it was also seen that the RNFL thickness was inversely correlated with the number and duration of migraine attacks seen in the migraine with aura compared to the migraine without aura which did not show this significant inverse correlation. The use of fMRI to evaluate the severity of migraine with aura patients determined that the reduction of the RNFL layer was related to the visual aura process in which inhibition of neuronal cell spreading was exhibited [12]. The authors infer that the changes of the RNFL compared to other regions of the retina were because it was thinner than that of other regions and thus it is particularly susceptible to neuronal degeneration.
Lastly, in Yurtoğulları et al., where mostly women exhibited migraine episodes, the macular RNFL thickness was significantly thinner in the migraine with aura group compared to the migraine without aura group [13]. Furthermore in another section of the retinal nerve fibers, called the peripapillary superonasal RNFL, the thickness was found to be significantly thinner in the migraine with aura group than in the migraine without aura aura group. The authors also note that the most likely cause is that the RNFL is more sensitive and unstable than other components of the retina when an individual experiences an aura compared to the absence of an aura before a migraine.
Comparison of Retinal Vasculature With and Without Migraines
In, Karahan et al, the vascular density in different regions of the retina was tested to examine blood. Female patients experiencing a retinal migraine with aura show a statistically significant decrease in vascular density in the retinal microvascular layers. Namely, this decrease occurs in the macular deep capillary plexus. There is an increase in vascular density within the foveal avascular zone to potentially compensate for this reduction, t. Due to these noticeable changes in the retina, the researchers suggest the possibility of microangiopathy (small diseased blood vessels) being linked to the pathophysiology of the migraine. The primary occurrence of retinal migraines is caused by the constricted blood vessels supplying the eye, resulting in reduced blood flow to the eye.
Due to the underlying vascular nature of retinal migraines, several studies have proven that they are associated and comorbid with vascular diseases. Chong et al. point out that the migraines are in particular related to amaurosis fugax which occurs when interrupted blood flow occurs to one or both of the main retinal arteries, that is, the central retinal artery and ophthalmic artery [1]. This disease, however, largely stems from an embolus originating from a clot in the carotid arteries which may indicate that retinal migraines have a possibility to result from other underlying health causes [1]. Furthermore, Grosberg et al. in their review emphasize that the underlying pathophysiology of retinal migraines may be related to primary vascular dysregulation, a vascular disease that primarily hinders the eye’s ability to achieve homeostasis leading to an inability of the blood vessels to address the needs of the respective tissue which likely results in, but is not limited to, ischemia i.e., a reduction of blood flow in the vasculature [2]. The pathogenesis of monocular visual loss may be explained by this reduction of blood flow as it relates to retinal migraines. Due to the connection with other bodily systems, patients experiencing these migraines—particularly with aura—are at an increased risk of heart disease, ischemic stroke, and even mortality [7].
In one retrospective cohort study conducted by Al-Moujahed et al., blood flow efficiency to specific regions of the retina was examined in patients who previously had a migraine. It was found that those suffering from retinal migraines are at increased risk of retinal artery occlusion (RAO) compared to healthy controls [10]. This elevated risk of RAO subsequently increases the chances of temporary monocular visual loss. Furthermore, the research has shown that women experiencing retinal migraines with aura lead to a greater probability of RAO than those who reported no aura. Transient visual impairment is a commonly reported symptom of reduced blood flow to the retinal vasculature where 54% reported blurred vision during their migraine episodes with aura [10].
Migraines are known to asymmetrically affect the brain and the eyes, which is why infarction to both eyes as a result of vasoconstriction is rarely reported among patients. A more thorough analysis of the retina reveals that within the migraine groups (including both migraine with aura and migraine without aura), a 7% reduction rate was observed in the parafoveal region (the innermost part) of the retina [6].
As similarly seen in this cross-sectional study from Y. Chang et al., an increase of the FAZ was 0.300 ± 0.019 mm2 larger in the migraine with aura group than in the HC participants but no significant increase was seen between migraine with aura and HC participants [11]. Additionally, the superficial retinal capillary plexus (SCP), compared to the deep in Karahan et al, also exhibited a significant decrease between the migraine with aura and HC participants. These effects in patients with retinal migraine highlight the possibility of increased risk of stroke and cardiovascular disease due to the degenerative effect in the retinal vasculature.
Comparison of Retinal Vasculature in Migraine Patients With and Without Aura
In surveying the aforementioned and newly compiled articles, the authors compared the VD in patients exhibiting aura versus patients exhibiting no aura. It is important to note that the classification and diagnosis of retinal migraines are not dependent on whether the migraine aura is present or not.
In Al-Moujahed A, Tran EM, Azad A, et al., the effect of migraine with aura remains evident as the authors were 95% confident that patients with aura had a significantly higher chance for developing retinal artery occlusion than patients that exhibited no aura in their migraine episodes [10]. The authors also analyzed the different types of RAO, including central RAO (CRAO) and branch RAO (BRAO), and concluded with 95% confidence that the association was significant in patients with BRAO but not significant in CRAO. This leads to potential further discussion on how exactly CRAO affects the retinal arteries differently than the other types of RAO including BRAO.
Although Karahan et al. did not discuss the differences between migraine with aura and migraine without aura patients, Y. Chang et al. cross-sectional study which looked at the same retinal vascular defects in migraine patients did investigate the difference between migraine with aura and migraine without aura patients [7, 11]. They observed that the foveal VD was significantly lower in migraine with aura patients (7.8 ± 0.31 mm-1) than the migraine without aura patients (9.3 ± 0.44 mm-1) but no significant difference between migraine with aura patients and HC patients.
Lastly, in comparing female migraine patients with aura vs migraine patients without aura, Kızıltunç et al. concluded in their prospective cross-sectional study of 28 patients, that the choriocapillaris (the blood supply that connects to the retinal vasculature) had statistically significantly less VD for migraine with aura patients than that of migraine without aura and healthy control groups [8]. This apparent lack of VD particularly in the migraine with aura group, as the authors deduce, likely resulted from ischemic events in the migraine with aura. This source was not used in the above section because there were no significant results about patients exhibiting a migraine versus the healthy controls.
An overarching analysis of the compilation of articles indicates that although both retinal migraines, with or without aura, negatively affect the retinal vasculature and thus the retina as a whole, migraines with aura show a larger inhibition of the eye.
Discussion
Retinal Vasculature
The studies concluded that the occurrence of migraines is associated with conditions that narrow or constrict blood vessels that feed into the retina, causing a blockage of blood vessels [6-7, 10-11]. This apparent thinning of the blood vessels is a major contributor to the headache that occurs, especially in patients who have a migraine with aura versus without aura [6-7]. This discrepancy between patients with and without aura indicates that the visual field plays a large role in the severity of the migraine, showing more significant alterations to the vascular retina in the presence of aura [10]. Chong et al. concluded that in retinal migraine patients with aura, the attacks originate in the central visual field before further spreading at a speed of 2-3 mm/min [1]. Possible implications of these findings reveal that blood thinners or neutralizing the clots using invasive strategies could be a source for future research.
Retinal Nerve Fiber Layer
Studies conclude that RNFL thickness is an apparent degenerative issue seen among different groups of retinal migraine participants, but there is a general lack of consensus and information to conclude any specific type of treatment available for a general population [9, 11-13]. As explained in the Reggio et al. (2016) observational and cross-sectional study, future research with MRI will provide researchers with a more in-depth understanding of the RNFL’s effects on the brain, and how white matter may contribute to the cognitive functions of migraine patients [9]. Interestingly enough, the researchers propose that the NSAIDs and triptans taken by the migraine overuse headache (MOH) participants negatively affect the condition of their retina, which may have minorly skewed their data in terms of RNFL thickness. Even though there was no major impact, the researchers note that the contribution of these drugs should not be ruled out which warrants further studies to investigate their impact [9]. However, Yurtoğulları et al. note that in further studies, understanding the different subcomponents of the RNFL among other sections of the retina with a larger sample size can contribute to a better understanding of the pathophysiology of migraines and more importantly, what modes of treatment can best cater to ganglion cell death [13].
Limitations
The rare nature of retinal migraines led to some key limitations that would not have been present otherwise including sample size and a general lack of studies. In the peer-reviewed journals, there were noticeably many more reviews and case reports that were on retinal migraines (and the surrounding terms) than actual studies performed on a cohort of patients. This lack of studies may be attributed to the rarity of the disorder and that it would be unethical and improper to diagnose a patient based on a few similarities with the disorder without ruling out more common disorders. For example, monocular vision impairment is a key factor of retinal migraines but, if the patient is not exhibiting these in short bursts and is not due to an underlying migraine, the patient cannot be used in the study. Another key limitation is the fact that the amount of patients tested was not extensive and for the data to become representative of the population (all women with retinal migraines) further studies should attempt to gather a larger sample. Many of the articles that were extensively analyzed and integrated into this literature review used a small sample size because the patients were simply not available due to the rare nature of diagnosing a patient experiencing retinal migraines. As time progresses, knowledge of retinal migraines and migraines in general will become clearer and thus authors will be able to make conclusions with more confidence.

About the Author: Mustafa Alesmail
Mustafa Alesmail is a third-year UC Davis undergraduate student pursing a Human Biology degree to which he ultimately plans to obtain a medical degree from his deep-rooted interest in medicine. Mustafa’s major ambition to write this paper stems from the fact that his mother has suffered from chronic migraines and after shadowing an ophthalmologist, he decided to combine both interests into a research paper looking at the effects of retinal migraines in regards to the blood vessels and nerve fibers that lead to the retina. Retinal migraines, an extremely rare eye condition, leads to severe blindness in one eye that may last up to an hour per episode. Mustafa details in his paper that the deficiency in vision largely stems from the irregularities in the structure of the retina that impact blood flow and neuronal signaling. Mustafa hopes that by reading his paper, he can shed light on the seemingly unknown nature of migraines but notes that migraines remain a heavy topic of discussion that warrants further research to find reliable and valid interventions.
References
Chong YJ, Mollan SP, Logeswaran A, Sinclair AB, Wakerley BR. 2021. Current Perspective on Retinal Migraine. Vision [Internet]. 5 (3). doi:https://doi.org/10.3390/vision5030038.
Grosberg BM, Veronesi M. 2024. Retinal migraine. In: Swanson JW, Matharu M. Handbook of Clinical Neurology. 199:381-387. doi:https://doi.org/10.1016/B978-0-12-823357-3.00012-4.
Maher ME, Kingston W. 2021. Retinal Migraine: Evaluation and Management. Current Neurology and Neuroscience Reports [Internet].21 (7). doi:https://doi.org/10.1007/s11910-021-01122-1.
Lai J, Esma D. 2020. Migraine Aura: Updates in Pathophysiology and Management. Current Neurology and Neuroscience Reports [Internet]. 20 (6). doi:https://doi.org/10.1007/s11910-020-01037-3.
Abdelghaffar M, Hussein M, Thabet NH, Elshebawy H, Daker LI, Soliman SH. 2022. The potential impact of migraine headache on retinal nerve fiber layer thickness. The Egyptian Journal of Neurology, Psychiatry, and Neurosurgery [Internet]. 58 (1). doi:https://doi.org/10.1186/s41983-022-00570-x.
Lin X, ZhongQuan Y, Zhang X, et al. 2021. Retinal nerve fiber layer changes in migraine: a systematic review and meta-analysis. Neurological Sciences [Internet]. 42 (3):871-881. doi:https://doi.org/10.1007/s10072-020-04992-4.
Karahan M, Erdem S, Ava S, Kaya AA, Demirtas AA, Keklikci U. 2021. Evaluation of retinal and optic nerve vasculature by optic coherence tomography angiography in Migraine with Aura. Journal Français d’Ophtalmologie [Internet]. 44 (9):1396-1402. doi:https://doi.org/10.1016/j.jfo.2021.02.018.
Bingöl Kızıltunç, P., Özcan, G., Özer, F. et al. 2020. Evaluation of retinal vessel density and choriocapillaris flow in migraine patients with and without aura. Graefes ArchClinExpOphthalmol[Internet].258:2517–2521. https://doi.org/10.1007/s00417-020-04805-6.
Reggio E, Chisari CG, Ferrigno G, et al. 2017. Migraine causes retinal and choroidal structural changes: evaluation with ocular coherence tomography [Internet]. J Neurol. 264 (3):494-502. doi:10.1007/s00415-016-8364-0.
Al-Moujahed A, Tran EM, Azad A, et al. 2021. Risk of Retinal Artery Occlusion in Patients with Migraine. Am J Ophthalmol [Internet]. 225:157-165. doi:10.1016/j.ajo.2020.11.004.
Melinda Y. Chang, Nopasak Phasukkijwatana, Sean Garrity, Stacy L. Pineles, Mansour Rahimi, David Sarraf, Mollie Johnston, Andrew Charles, Anthony C. Arnold. 2017. Foveal and Peripapillary Vascular Decrement in Migraine With Aura Demonstrated by Optical Coherence Tomography Angiography. Invest. Ophthalmol Vis. Sci. [Internet]. 58(12):5477-5484. https://doi.org/10.1167/iovs.17-22477.
Ran Ao, Rongfei Wang, Mo Yang, Shihui Wei, Xuehui Shi, Shengyuan Yu. 2019. Altered Retinal Nerve Fiber Layer Thickness and Choroid Thickness in Patients with Migraine. Eur Neurol [Internet]. 80 (3-4):130–137. https://doi.org/10.1159/000494671.
Yurtoğulları, Şükran & Erbahçeci Timur, İnci Elif & Eyidoğan, Demet. 2021. Retinal Thickness Alterations in Patients with Migraine. Turkish Journal Of Neurology [Internet]. 27: 69-74. 10.4274/tnd.2020.06791.
