By Lo Tuan, Neurobiology, Physiology, and Behavior and Managerial Economics, ’17
Author’s Note:
“I chose to write this paper because I have a family member who suffers from TTH and expanding my knowledge of the topic through researching and writing empowered me to play a more active role in assisting my family with addressing such medical condition.”
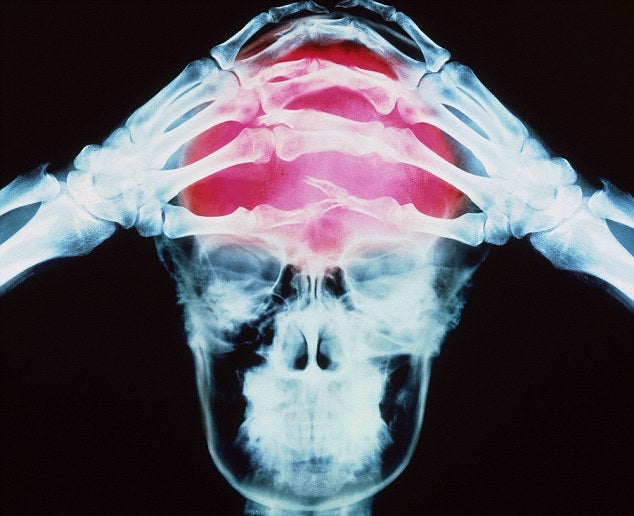
As the most common headache, tension-type headache (TTH) affects approximately 80 percent of the population annually and is the second-most prevalent disorder in the world (Taylor 2016a). TTH is characterized by generalized, nonthrobbing pain in the absence of migraine-induced incapacity, nausea, or photophobia. Tension-type headache normally produces mild to moderate pain often described as viselike. It originates bilaterally in the occipital or frontal lobes and extends to the rest of the brain. TTH occasionally causes unilateral or pulsating pain. Two prominent features distinguish TTH from migraine. First, TTH does not lead to nausea and vomiting. Second, it is not made worse by physical activity, light, sounds, or smells (Silberstein 2014).
Classification
There are two types of TTH categorized by attack frequency: episodic TTH refers to the condition in which patients suffer headaches at a rate of less than 15 headache days a month, and chronic TTH involves 15 or more headache days a month. Both types may contribute to significant disability, especially when patients also suffer from migraine, comorbid depression, or anxiety (Taylor 2016b). Episodic TTH is further broken down to two subtypes: frequent episodic (1 to 14 headache days per month) and infrequent episodic (less than 1 headache day per month). The duration of episodic headaches ranges from half an hour to several days. Episodic TTH typically starts several hours after waking and increases in intensity as the day progresses. The pain intensity associated with this type of TTH is rarely sufficient to disrupt sleep. Chronic TTH can be triggered by sleep disturbances, stress, temporomandibular joint dysfunction, neck pain, and eyestrain (Silberstein 2014). This type of TTH varies in intensity throughout the day but is almost always present.
The classification of these three types of TTH is critical, as each has its own distinct underlying pathophysiology, influence on daily functioning, and treatment methods. For example, peripheral mechanisms are more closely associated with episodic TTH, while central mechanisms are more relevant in chronic TTH. More specifically, the development of episodic TTH is contingent upon the peripheral activation or sensitization of myofascial nociceptors, whereas the transition from episodic to chronic TTH relies on the sensitization of pain pathways in the central nervous system established through prolonged exposure to nociceptive stimuli from pericranial myofascial tissues (Bendtsen et al. 2015). With regard to the treatment of these different types of TTH, infrequent episodic TTH usually calls for an acute symptomatic approach, while frequent episodic TTH and chronic TTH require prophylactic interventions. Each type of TTH can be additionally sorted based on the concurrent presence or absence of pericranial muscle tenderness.
Neurologic consultation normally only follows lengthy experience of headaches. In particular, TTH is the most prevalent type of primary headache in the general population. Despite the overall high prevalence of TTH, most patients with TTH have the infrequent episodic subtype. Some physicians argue that this type of TTH is not a disease. Instead, they regard it as a normal phenomenon that does not call for medical attention. Since most individuals with TTH have infrequent, mild headaches, only a small percentage of the affected population seek medical care to address such condition. Women have a slightly higher probability of experiencing TTH than men. This asymmetry is especially conspicuous in frequent episodic and chronic tension-type headaches.
Tension-type headache was previously known by different names, including stress or tension headache, muscle-contraction headache, psychomyogenic headache, and psychogenic headache (Taylor 2016a). The term tension was initially chosen to reflect tension headache’s suspected etiology: excessive stress or tension leading to muscle contraction. Traditionally, it was thought that sustained contracture of pericranial muscles causes TTH, though the notion is no longer accepted.
Pathophysiology
Although the precise mechanisms through which TTH develops remain unknown, the pathogenesis of TTH most likely involves multiple factors. Different factors have varying degrees of influence over the development of TTH, depending on the type. For example, environment plays a greater role in the development of episodic TTH than chronic TTH. In contrast, genetic factors have more of an impact on the development of chronic TTH than episodic TTH. Nitric oxide has been identified as a potential molecular trigger for pain associated with TTH. Tension-type headache’s underlying pain mechanisms are likely dynamic to account for the observed diversity in frequency and intensity of headache attacks. They vary not only between individuals, but also within individuals over time from one attack to the next.
Diagnosis
The diagnosis of TTH is reached through a clinical evaluation consisting of symptoms assessment and a physical examination that includes a neurologic examination. There are no diagnostic tests specific for TTH. During the evaluation, effort is made to identify potential triggers for chronic tension-type headache in order to devise targeted treatment plans. In addition, practitioners look out for differences that set TTH apart from a forme fruste of migraine to avoid misdiagnosis. These headaches possess certain features of migraine and certain features of tension-type headache, but they differ from TTH in their responsiveness to migraine-specific drugs. Physicians should be cautious about diagnosing severe headaches as TTH, because severe tension-type headaches are rare. Due to extensive symptom overlap between TTH and secondary headaches, it is essential for doctors to closely observe the temporal pattern of headaches to reach an accurate diagnosis.
Patients with TTH usually have normal results from physical and neurologic examinations, blood work, brain imaging with CT or MRI scans, and spinal fluid analyses (Taylor 2016a). The most prominent abnormal finding in patients with TTH is increased pericranial muscle tenderness, or muscle tenderness in the head, neck, or shoulders. Pericranial muscle tenderness acts as a signal for the intensity and frequency of TTH attacks and generally worsens during a headache. The presence or absence of pericranial muscle tenderness can be discerned through an examination by manual palpation. Manual palpation describes the application of firm pressure with the second and third fingers making small rotating movements on the pericranial muscles, including the frontal, temporal, masseter, pterygoid, sternocleidomastoid, splenius, and trapezius muscles (Taylor 2016a).
Because pure TTH is a rather featureless headache, practitioners need to be attentive of all possible diagnoses when examining a patient. In particular, physicians encounter diagnostic challenges when patients present with atypical or missing symptoms, symptoms that overlap with other types of headaches, or an incomplete self-report of symptoms. When a patient with a normal physical examination displays a stable pattern of episodic and disabling headaches, practitioners should consider the diagnosis of migraine if there is no evidence that suggests otherwise.
Another condition that closely resembles TTH is brain tumor headache, though it is rarer. Its features are typically nonspecific and dependent upon tumor location, size, and rate of growth (Taylor 2016a). Brain tumor headache is generally bilateral though it can be restricted to the side of the tumor. A third type of headache that shares similar features with TTH is medication overuse headache (MOH). MOH is a secondary headache that normally results from treating an episodic headache disorder such as TTH with frequent and excessive amounts of acute symptomatic medications. Therefore, practitioners should suspect MOH in patients who adopt a pharmacologic approach to treatment. For patients with unilateral pain, cervicogenic headache is a probable diagnosis. Pain from cervicogenic headache ranges from moderate to severe intensity and radiates from occipital to frontal regions. It can be exacerbated by head movements and is nonlancinating.
Treatment and Prevention
Treatment of TTH consists of two major components: analgesics, and behavioral and psychologic interventions. Additionally, some drugs used to prevent migraine such as amitriptyline are also effective in preventing chronic tension-type headache (Silberstein 2014). For most cases of tension-type headaches, over-the-counter analgesics such as aspirin and acetaminophen provide significant relief. Behavioral and psychologic interventions involve relaxation and stress management techniques. These treatment methods are especially potent when used in conjunction with drug therapy.
Patients with frequent episodic or chronic TTH should consider preventive treatment as a way to alleviate disabling pain. Preventive treatment of TTH involves both drugs and nonpharmacologic approaches such as behavioral and cognitive therapies. Many of these preventive measures are derived from those used for migraine because the two conditions share significant overlap. These efforts aim to reduce attack frequency, severity, and duration; improve responsiveness to treatment of acute attacks; ameliorate function; and decrease disability (Taylor 2016b).
The pharmacologic approach typically involves prescription of tricyclic antidepressants such asamitriptyline (Semenov 2015). Other potential candidates for TTH prophylaxis include serotonin-norepinephrine reuptake inhibitors such as mirtazapine and venlafaxine, and anticonvulsants such as gabapentin and topiramate (Banzi et al. 2015). Practitioners should be cautious about prescribing these medications because current clinical data lacks sufficient evidence to support their efficacy.
Nonpharmocologic preventive treatments include biofeedback, relaxation, and cognitive-behavioral therapy. They aim to identify and remove behavioral headache triggers, thereby preventing headaches. A combination of pharmacologic and nonpharmocologic approaches can be an effective treatment method. For example, combined tricyclic antidepressant and stress management therapy is recommended for patients with frequent episodic or chronic TTH. Those that prefer pharmacologic intervention over behavioral therapy should consider tricyclic therapy with amitriptyline. In contrast, for patients who wish to avoid or cannot tolerate pharmacologic intervention, electromyography (EMG) biofeedback in conjunction with relaxation therapy is a viable treatment option.
Bibliography
Banzi R, Cusi C, Randazzo C, Sterzi R, Tedesco C, Moja L. 2015. Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotoninnorepinephrine Reuptake Inhibitors (SNRIs) for the Prevention of Tension-Type Headache in Adults. The Cochrane Library [Internet]. [cited 2016 Mar 6]; 5. Available from: https://vpn.lib.ucdavis.edu/,DanaInfo=ucelinks.cdlib.org, Port=8888+sfx_local?sid=Entrez:PubMed&id=pmid:25931277
Bendtsen L, Ashina S, Moore A, Steiner TJ. 2015. Muscles and Their Role in Episodic Tension-Type Headache: Implications for Treatment. European Journal of Pain [Internet]. [cited 2016 Mar 6]; 20(2): 166-175. Available from: https://vpn.lib.ucdavis.edu/,DanaInfo= ucelinks.cdlib.org,Port=8888+sfx_local?sid=Entrez:PubMed&id=pmid:26147739
Semenov IA. 2015. Tension-Type Headaches. Disease-a-Month [Internet]. [cited 2016 Mar 6]; 61(6): 233-235. Available from: https://vpn.lib.ucdavis.edu/science/article/pii/, DanaInfo=www.sciencedirect.com+S0011502915000450
Silberstein SD. 2014. Tension-Type Headache [Internet]. Kenilworth (NJ): Merck & Co., Inc.; [cited 2016 Mar 6]. Available from: http://www.merckmanuals.com/professional/ neurologic-disorders/headache/tension-type-headache
Taylor FR. 2016a. Tension-Type Headache in Adults: Pathophysiology, Clinical Features, and Diagnosis [Internet]. Waltham (MA): UpToDate; [cited 2016 Mar 6]. Available from: https://vpn.lib.ucdavis.edu/contents/,DanaInfo=www.uptodate.com+tension-type-headache-in-adults-pathophysiology-clinical-features-and-diagnosis?source=search_result&search= tension+type+headache&selectedTitle=2~74
Taylor FR. 2016b. Tension-Type Headache in Adults: Preventive Treatment [Internet]. Waltham (MA): UpToDate; [cited 2016 Mar 6]. Available from: https://vpn.lib.ucdavis.edu/ contents/,DanaInfo=www.uptodate.com+tension-type-headache-in-adults-preventive-treatment?source=search_result&search=chronic+headache& selectedTitle=4~150