By Daniel Erenstein, Neurobiology, Physiology, and Behavior, ‘20
Author’s Note: One of the major assignments in my Writing in Science (UWP 104E) course was a literature review on some current topic of scientific interest. The process involved in understanding prior research on a topic and in predicting a field’s future directions was challenging. Along the way, I often found myself lost in a world of complicated scientific jargon. In the end, it was a personal story that provided the inspiration I needed for this article. Worldwide, more than 70,000 people have cystic fibrosis, and there are over 30,000 patients in the United States alone. Mary Frey is one of them, and she chronicles her life alongside Peter, her husband, and Ollie, her service dog, in daily vlogs on their YouTube channel. With “The Frey Life,” I was reminded that scientific research, which might sometimes seem removed from the realities of life, should be rooted in the spirit of helping people. This message guided and energized my research on cystic fibrosis. I thank Dr. Brenda Rinard for her valuable instruction, which shaped this review article throughout the writing process.
Abstract
Personalized medicine, a recent addition to the growing toolkit of clinical physicians, has developed within the last decade into a practical strategy for effectively treating diseases. One such disease, cystic fibrosis, serves as an excellent window into the field of personalized medicine. The following review article examines the current state of cystic fibrosis research, in the process detailing recent studies on the correlations, or lack thereof, between mutant genotypes and disease phenotypes. Knowledge of these relationships is incomplete, necessitating the need for further patient population studies and drug treatment tests. Toward the end of the article, studies on the effects of certain cystic fibrosis drugs currently in the pipeline are presented. With future findings, clinical treatment of cystic fibrosis can be significantly improved by our foundational understanding of the effects of personalized medicine on the individual. Treatments targeting cystic fibrosis genotypes are a promising alternative to the existing and often unsuccessful clinical methodologies, which place an emphasis on the symptoms of the disease.
Keywords: personalized medicine; precision medicine; cystic fibrosis (CF); cystic fibrosis transmembrane conductance regulator (CFTR) gene; Clinical and Functional Translation of CFTR (CFTR2) database; ΔF508 mutations; rare mutations (RMs).
Introduction
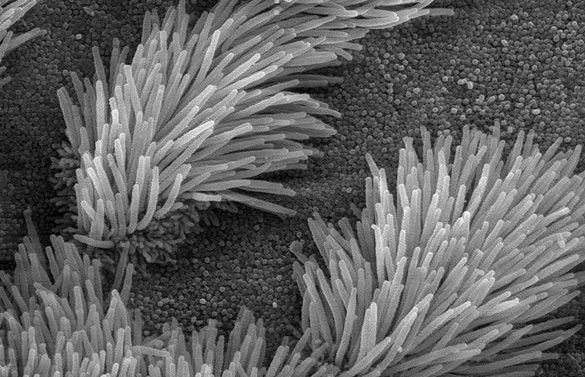
Cystic fibrosis—a genetically-inherited, life-threatening condition that infects the lungs, the respiratory system, and the digestive system—affects over seventy thousand people worldwide according to the Cystic Fibrosis Foundation Patient Registry (1). The disease is caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, which controls the expression of chloride and bicarbonate ion channels in the plasma membrane of respiratory and epithelial cells (2). An imbalance in the number of ion channels or a decrease in the probability of open channels triggers several physiological issues, including mucus buildup, inflammation of lung tissue, and bacterial infection (2, 3). Medical approaches with a focus on treating these symptoms, among others, have proven insubstantially effective in slowing the development of the disease (2).
This literature review explores the relationship between CFTR genotypes and corresponding phenotypes as described by recent research. We highlight the influence of CFTR mutations in resulting cystic fibrosis phenotypes, with a specific focus on ΔF508 and other rare mutations. Despite the present body of research into these genetic relationships, the extent of the correlation between cystic fibrosis genotype and phenotype is largely unknown. A thorough and complete understanding of the mechanisms by which genotype influences phenotype is crucial to the development of personalized approaches to medical treatment. Through an analysis of the underlying genotype-to-phenotype relationships, we present an evaluation of existing methods of disease diagnosis, prognosis, and treatment. Future research, if effectively designed and executed, could potentially reveal new avenues toward successful, targeted treatments of cystic fibrosis.
Correlations between Genotype and Phenotype
The origins of modern research into the correlations between cystic fibrosis genotype and phenotype are often attributed to Kerem et al.’s 1990 analysis of the most common CFTR mutation, ΔF508, named for the amino acid position that the corresponding DNA base pair deletion affects (2, 4, 5, 6). A thorough study of cystic fibrosis patients at the Hospital for Sick Children (Toronto) from 1977 to 1990 followed patients from diagnosis, evaluating each individual’s pancreatic function, testing for the presence of pulmonary disease, assessing growth and nutritional status, and measuring sweat chloride levels (4). In only one percent of homozygous ΔF508 patients was pancreatic function sufficient in the absence of added enzymes, in stark contrast to the twenty-eight percent of heterozygous patients and sixty-four percent of patients with other mutations who experienced sufficient function in their pancreas (4). The study’s conclusion that differences in phenotypic intensity are mirrored by differences in cystic fibrosis genotypes, combined with earlier research into phenotypic expression of mutant genotypes in C. elegans roundworms, is convincing evidence that genotype and phenotype are inextricably related (4, 7).
Past research has discovered strong correlations between the presence of ΔF508 mutations in a genotype and the intensity of corresponding disease phenotypes (5). Pancreatic insufficiency as related to the progression of cystic fibrosis seems to be dependent on genotype (5). The severity of cystic fibrosis symptoms is markedly higher for pancreatic-insufficient patients, and those with pancreatic insufficiency typically have severe CFTR mutations on both alleles (5).
Additional support for this correlational hypothesis is provided by existing research. Classifications of high-risk and low-risk genotypes, if properly assigned through an evaluation of phenotypic disease severity and protein production levels, are a useful tool for predicting disease progression (8, 9). Ninety-three percent of individuals with CFTR mutations recorded in the U.S. Cystic Fibrosis Foundation (CFF) patient registry were classified as having a high-risk genotype. These individuals with a high-risk genotype were 2.25 times less likely to survive than the seven percent of individuals with a low-risk genotype (8). In a further exploration of the data available from the Cystic Fibrosis Foundation, patient survival was correlated with sweat chloride concentrations and again with genotypic-risk groups: as sweat chloride concentration and risk group of the genotype increased, survival decreased (9). Patients with at least partially functional CFTR proteins experienced prolonged survival in comparison to those with fully non-functional CFTR proteins (9). In several studies, effects of phenotypic factors on survival were shown to be statistically insignificant, linking defective genotypes directly to disease severity and transforming gene sequences into a reliable forecaster of survival likelihood (3, 7, 8).
However, current consensus on the correlational hypothesis is limited by a lack of genetic data from patients with unidentified or rare CFTR mutations. Information on rare mutations (RMs) is absent from the Clinical and Functional Translation of CFTR (CFTR2) database, which catalogues the currently-known CFTR mutations and reports associations between the mutations and corresponding phenotypes (6). This lack of data presents medicine with challenges when trying to diagnose and treat patients whose gene sequences include RMs. Additionally, the range of disease-related symptoms seen in patients with cystic fibrosis cannot be explained simply by mutations in the CFTR gene (2, 6, 10, 11, 12). In the following section, alternative correlational factors and diagnostic methods are discussed. These variables could potentially prove to be more reliable predictors of disease diagnosis and progression, or explain more fully the mechanisms behind genotype-to-phenotype relationships.
Genetic Modifiers, Environmental Variables, and Other Factors
Genotyping of CFTR sequences in the cystic fibrosis gene locus is certainly not the only clinical method of disease diagnosis. As a result of the incomplete data described above, research has suggested that sweat chloride concentration and nasal potential difference measurements are more effective tools in clinical diagnosis of cystic fibrosis (6, 13). Arguably, a number of phenotypic factors might influence the responses of individual patients to certain CFTR mutation-specific therapies. The effects of CFTR mutations can be noticed at any age in varying degrees of intensity: for any given age and genetic background, phenotypes can vary (5). While many studies take exhaustive steps to ensure that differing levels of disease severity are indeed caused by genetic variation, there exist significant limitations to research that makes conclusions in favor of direct genotype-to-phenotype correlations (at least in the context previously discussed). Environmental variables, such as poor nutrition, might very well affect pancreatic insufficiency, just as the variability in pulmonary function likely affects the severity of cystic fibrosis disease symptoms (5, 6).
In addition to the above-mentioned phenotypic symptoms of cystic fibrosis, genetic modifiers are a potential explanation for how the same clinical treatment can induce different reactions from individuals with the same CFTR mutations (2). An assessment of the Canadian cystic fibrosis population analyzed the pleiotropic effects of genetic modifiers on patient survival and disease prognosis (12). Pleiotropic modifiers make a complete understanding of the complex relationships between cystic fibrosis genotype and phenotype difficult to achieve (12). Further research demonstrates the role that multiple modifier gene loci play in the severity of cystic fibrosis-related lung disease (10). The complications caused by these genetic modifiers create significant obstacles in the process of formulating correlations between genotype and phenotype. The resulting deficit in molecular and mechanical understanding necessitates further research, the specifics of which are elucidated in the next section.
Recent and Future Developments of Personalized Medicine
Future progress in personalized medicine requires from the field of cystic fibrosis research the development of effective models and the experimental evaluation of novel cystic fibrosis treatments. Many of the current treatments for cystic fibrosis, including antibiotics for lung infections and mucociliary clearance (MCC), inadequately slow the development of the disease and only marginally improve the likelihood of surviving longer (2). The following section will highlight current research and recommended strategies to direct the field of cystic fibrosis closer to clinically successful diagnostic approaches and treatment methods.
Additional research and mutation-cataloguing is needed to strengthen the quality of clinical diagnoses. Genetic analysis loses its value in diagnosing cystic fibrosis if identified rare mutations are uncharacterized by CFTR databases (14). To improve the cataloguing of rare mutations in CFTR databases, centers for cystic fibrosis should continue to record this data (6). To understand the disease-causing potential of rare mutations, data must also be catalogued from a larger population. This is the current aim of the developing CFTR3 database (6).
Much of the current cystic fibrosis research concerns the evaluation of pharmaceutical treatments for the disease. One such drug is ivacaftor, developed to target the functional defects caused by CFTR mutations through the activation of CFTR (3). Ivacaftor is one of the more promising treatments for cystic fibrosis, as evidenced by sweat chloride tests in cystic fibrosis patients with the G551D mutation (13). Char et al. researched the effects of ivacaftor on individuals with G551D/ΔF508 or R117H-5T mutations in their genotype (3). The study established a methodology for testing the effect of a mutation by using the ratio of CFTR-dependent “C-sweat” secreted from an individual to CFTR-independent “M-sweat” secreted from that same individual (3). To record sweat ratios, CFTR-independent M-sweating was induced with methacholine and then experimentally inhibited, triggering the production of CFTR-dependent C-sweating (3). Usually, sweat-chloride concentration tests are unreliable indicators of functioning CFTR levels, but C-sweat/M-sweat testing allows for the control of variations in sweat volume between two patients, eliminating some of the variables encountered in the previous section (3). Since the process that generates C-sweat is dependent on the functionality of CFTR, greater C-sweat/M-sweat ratios can be interpreted to indicate that the CFTR protein was functioning at a higher level (3). The presence of ivacaftor prompted larger sweat ratios (3). Therefore, ivacaftor is considered a useful treatment for certain CFTR mutations. Other pharmaceutical drugs are currently undergoing development, including some that have progressed to clinical trials (2).
The mechanisms behind genetic modifiers and their influence on disease intensity is not yet fully understood, so these pathways have not been utilized in pharmaceutical medicine to date. A more complete knowledge of these mechanisms might provide insight into precise medical treatment plans or suggest molecular pathways that can be targeted by drugs (2, 12, 15).
While past and present research has realized significant advances in the prediction of patient-specific reactions to pharmaceutical therapies, in vivo examinations of CFTR’s response to drugs are still required to evaluate the effects of drugs on a cystic fibrosis patient (2). In vitro assays are also useful, but must consider the typical internal environment in lungs afflicted with cystic fibrosis, incorporating this into the experimental design (2). A greater depth of in vivo and in vitro research is required to develop an ideal personalized medicine model for patients, one that eases the phenotypic effects of cystic fibrosis mutations by targeting the CFTR gene sequence, or corresponding protein, itself.
Conclusion
With these recent findings in mind, the most effective personalized medicine method in practice is likely a synthesis of various gene therapies and different treatments that target physiological symptoms of disease. Based on the current body of research, it is widely understood and accepted that cystic fibrosis phenotypes are influenced by CFTR mutations, but in what way and to what extent remains unclear. Furthermore, disease phenotypes cannot be explained simply as a result of CFTR mutations. Before drawing experimental conclusions or designing clinical methods for treatment, any well-rounded and complete analysis of disease severity should consider genetic modifiers, environmental variables, and the effects of other phenotypic factors. On a larger scale, the correlations between genotype and phenotype described throughout this literature review seem to accurately predict population dynamics, but until further genetic analyses, clinical experiments, and pharmaceutical research can be completed, the present state of cystic fibrosis research advises against the specific diagnosis of an individual on the basis of genotype-to-phenotype correlations.
Works Cited
-
About Cystic Fibrosis [Internet]. 2017. Bethesda (MD): Cystic Fibrosis Foundation; [cited 2017 Nov 13]. Available from https://www.cff.org/What-is-CF/About-Cystic-Fibrosis/
-
Deborah M. Cholon, Martina Gentzsch. 2017. Recent progress in translational cystic fibrosis research using precision medicine strategies. J Cyst Fibros. Article in Press.
-
Jessica E. Char, Marlene H. Wolfe, Hyung-ju Cho, Il-ho Park, Jin Hyeok Jeong, Eric Frisbee, Colleen Dunn, Zoe Davies, Carlos Milla, Richard B. Moss, et al. 2014. A little CFTR goes a long way: CFTR-dependent sweat secretion from G551D and R117H-5T cystic fibrosis subjects taking ivacaftor. PLOS One. 9(2):88564.
-
Eitan Kerem, Mary Corey, Bat-sheva Kerem, Johanna Rommens, Danuta Markiewicz, Henry Levison, Lap-Chee Tsui, Peter Durie. 1990. The relation between genotype and phenotype in cystic fibrosis – analysis of the most common mutation (ΔF508). N Engl J Med. 323(22):1517-1522.
-
Carol Durno, Mary Corey, Julian Zielenski, Elizabeth Tullis, Lap-Chee Tsui, Peter Durie. 2002. Genotype and phenotype correlations in patients with cystic fibrosis and pancreatitis. Gastroenterology. 123(6):1857-1864.
-
E. De Wachter, M. Thomas, S. S. Wanyama, S. Seneca, A. Malfroot. 2017. What can the CF registry tell us about rare CFTR-mutations? A Belgian study. Orphanet J Rare Dis. 12(42).
-
Victoria Vu, Adrian J. Verster, Michael Schertzberg, Tungalag Chuluunbaatar, Mark Spensley, Djina Pajkic, G. Traver Hart, Jason Moffat, Andrew G. Fraser. 2015. Natural variation in gene expression modulates the severity of mutant phenotypes. Cell. 162(2):391-402.
-
Edward F. McKone, Christopher H. Goss, Moira L. Aitken. 2006. CFTR genotype as a predictor of prognosis in cystic fibrosis. Chest. 130(5):1441-1447.
-
Edward F. McKone, Priscilla Velentgas, Anna J. Swenson, Christopher H. Goss. 2015. Association of sweat chloride concentration at time of diagnosis and CFTR genotype with mortality and cystic fibrosis phenotype. J Cyst Fibros. 14(5):580-586.
-
Harriet Corvol, Scott M. Blackman, Pierre-Yves Boëlle, Paul J. Gallins, Rhonda G. Pace, Jaclyn R. Stonebraker, Frank J. Accurso, Annick Clement, Joseph M. Collaco, Hong Dang, et al. 2015. Genome-wide association meta-analysis identifies five modifier loci of lung disease severity in cystic fibrosis. Nat Commun. 6(8382).
-
Lei Sun, Johanna M. Rommens, Harriet Corvol, Weili Li, Xin Li, Theodore A. Chiang, Fan Lin, Ruslan Dorfman, Pierre-François Busson, Rashmi V. Parekh, et al. 2012. Multiple apical plasma membrane constituents are associated with susceptibility to meconium ileus in individuals with cystic fibrosis. Nat Genet. 44(5):562-569.
-
Weili Li, David Soave, Melissa R. Miller, Katherine Keenan, Fan Lin, Jiafen Gong, Theodore A. Chiang, Anne L. Stephenson, Peter Durie, Johanna M. Rommens, et al. 2014. Unraveling the complex genetic model for cystic fibrosis: pleiotrophic effects of modifier genes on early cystic fibrosis-related morbidities. Hum Genet. 133(2):151-161.
-
Verena I. Seliger, David Rodman, Fredrick Van Goor, Andreas Schmelz, Peter Mueller. 2013. The predictive potential of the sweat chloride test in cystic fibrosis patients with the G551D mutation. J Cyst Fibros. 12(6):706-713.
-
Patrick R. Sosnay, Danieli B. Salinas, Terry B. White, Clement L. Ren, Philip M. Farrell, Karen S. Raraigh, Emmanuelle Girodon, Carlo Castellani. 2017. Applying cystic fibrosis transmembrane conductance regulator genetics and CFTR2 data to facilitate diagnoses. J Pediatr. 181:S27-S32.
-
C. Castellani, H. Cuppens, M. Macek Jr., J. J. Cassiman, E. Kerem, P. Durie, E. Tullis, B. M. Assael, C. Bombieri, A. Brown, et al. 2008. Consensus on the use and interpretation of cystic fibrosis mutation analysis in clinical practice. J Cyst Fibros. 7(3):179-196.