By Carly Cheung, Microbiology, ‘17
Author’s Note:
“The goal of this paper is to portray the multifunctionality of proteins involved in the cell and how interconnected one process is to another, even though two processes appear to be unrelated. I am fascinated by the system of signal transduction in our cells and admire how elaborate and complicated the network is. This is best shown by examining the two proteins, ATM and ATR, that are known for their functions in cell cycle regulation and DNA break repair. The paper explores the changes in their transduction pathways seen in mammals with cancer, metabolic diseases, and cardiovascular diseases.”
The phosphoinositide 3-kinase related kinase (PIKK) family members are important regulators of the cell cycle. All stages of the cell cycle–inactivity (G0), growth (G1), DNA synthesis (S), preparation for mitosis (G2), mitosis (M), and cytokinesis–are controlled by sensors that detect cues within the cell and messengers that pass on the signal (Bin-Bing, 2000). The transduced activities involve interactive gene regulations to relay a signal into an action. Ataxia telangiectasia-mutated (ATM) and Ataxia telangiectasia-mutated Rad3-related (ATR) are both signal transducers in the PIKK family that detect DNA breaks in the cell. It is essential that a cell detects DNA breaks to arrest the cycle and repair the DNA before continuing. ATM and ATR, like other kinases, phosphorylate active sites of specific downstream kinases, triggering a cascade of subsequent protein phosphorylation. Activated proteins can turn the transcription of genes on and off, as well as upregulate and downregulate expression of those genes, allowing a cell to actively respond to a direct cue. Research has found that ATM and ATR play roles in both regulating the cell cycle and initiating repair pathways to respond to DNA breaks (Bin-Bing, 2000).
Double stranded breaks activate ATM to phosphorylate the active site of checkpoint 1 (chk1), which activates subsequent proteins to phosphorylate the final protein in the pathway: p53. The ATM/p53 pathway is present in all phases of the cell cycle, possibly to ensure constant maintenance of the cell’s integrity. Experiments conducted by Espach and colleagues suggest that p53 protein is essential to ATM protein’s function. More is known about ATM because of the large array of diseases that result from a mutated ATM gene, such as immunodeficiency diseases, cancer, metabolic diseases, and cardiovascular diseases (Bin-Bing, 2000). The onset of such diseases highlights ATM’s critical role in homeostasis, cell cycle checkpoints, and apoptosis.
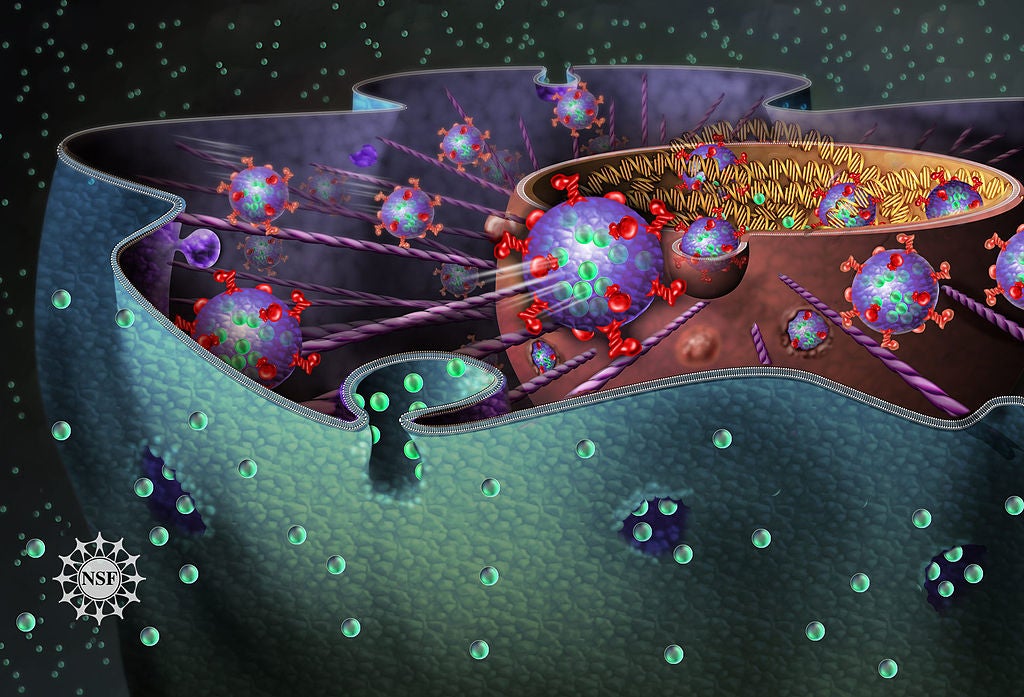
Patients either deficient in ATM, or possess a mutated ATM, display symptoms of metabolic syndrome such as insulin resistance in type 2 diabetes and high levels of the lipids or lipid containing molecules, like cholesterol, low density lipopolysaccharides, and triglycerides (Espatch, 2015). These observations suggest ATM plays a role in multiple cellular functions for stress regulation (Figure 1). Furthermore, scientists discovered that ATM is activated not only by double-stranded DNA breaks, but also by oxidative stress. ATM facilitates in reducing the stress with production of NADP+. Mice with increased ATM activation due to oxidative stress switches the cell’s glucose metabolism from glycolysis to the Pentose Phosphate Pathway. This pathway generates more nicotinamide adenine dinucleotide phosphate (NADP+), a cofactor known for its function as a reducing agent to oxidized compounds. When ATM is deficient in mice, it results in the activation of proteins that protect the cell, such as the vascular endothelial growth factor (VEGF). VEGF’s function is critical in blood vessel development and increases the transcription of myoglobin protein, which relieves stress by transferring oxygen to cells during exercise or other high stress situations. In addition, ATM’s deficiency is also directly involved in generation of these symptoms, by overproduction of GLUT1 and JNK1. GLUT1 promotes increased cell growth and the kinase JNK1 is involved in regulation of insulin signaling and fat production (Espatch, 2015). GLUT1 activates antioxidant responses as well as increases glucose uptake, ultimately contributing to an increase in insulin resistance. Interestingly, JNK1 phosphorylates the active site of a downstream protein that disrupts insulin signaling and acts as a transcription factor for lipoprotein lipase, an enzyme that generates cholesterol. The outcome of increased JNK1 transcription is insulin resistance and a build-up of cholesterol in the arteries. Further supporting the hypothesis that the negative effects seen are due to activation of JNK1 protein, mice deficient in JNK1 shows no signs of insulin resistance or obesity (Espatch, 2015). Mice that have lost one functional copy of ATM have elevated levels of cholesterol, low density lipopolysaccharides, and triglycerides. These discoveries opened up possible treatments for cardiovascular diseases and metabolic syndrome by synthetically increasing the activity of ATM protein to decrease activity of JNK1 protein.
Many cancer therapies build upon the idea of inhibiting the ATR/chk1 pathway in cancer cells. ATR responds to single-stranded DNA breaks and phosphorylates the active site of the chk1 protein. A cancer cell’s inability to repair its DNA breaks results in discontinuation of its life cycle and a quick accumulation of un-replicable DNA. Acknowledging its irreversible fate, the cancer cell undergoes apoptosis by the signal of un-replicable DNA. In an experiment where The ATR gene in mice were mutated, decreased growth rate of fibrosarcoma was seen (Fokas, 2014). Normal tissues received little to no impact even over a longer period of time, because cancer cells seem to only have the ATR/chk1 pathway, and no ATM pathway. In addition, the greater tendency of cancer cells to accumulate DNA replication stress, due to their characteristic abnormal growth, contributes to a potential drug’s specificity in targeting cancer cells instead of healthy cells (Fokas, 2014). When a drug inhibits the ATR/chk1 pathway in cancer cells and healthy cells, healthy cells remain viable because of their remaining functional ATM/p53 pathway, allowing the drug further specificity to target cancer cells (Durisova et al).
Another therapeutic application of ATR inhibition drugs is to use them in concert with chemotherapy against oncogenes. One example is the chemotherapeutic antimetabolite drug, Germacitabines, which is a nucleoside analog that is incorporated into the cell’s genome during replication, thereby terminating replication (Fokas, 2014). However, this mechanism requires an initiation of DNA replication by the tumor cell, which contributes to the number of natural occurrence of DNA breaks. The replication stress is a signal that naturally activates ATR/chk1 pathway to fix DNA breaks in order to continue the cancer cell’s life cycle. Therefore, this chemotherapeutic drug increases the function of ATR, promoting cell growth in tumor cells. However, when the antimetabolite is paired with ATR inhibition drugs to impair cancer cells’ ability to repair its broken DNA, the cancer cell becomes more sensitive to chemotherapy antimetabolites’ effects (Fokas, 2014). ATR inhibition drugs can enhance the efficiency of chemotherapy drugs.
The proteins involved in the ATR/chk1 and ATM/chk1 pathways construct an elaborate signal transduction network, not only to regulate the cell cycle, but also to ensure that the cell responds to the environment in a flexible manner. Phenotypes of cells that lack or have mutated ATR and ATM proteins highlight the importance of precise protein functions in every step of a pathway. An array of symptoms seen in type 2 diabetes, metabolic syndrome, and cancer, can be traced back to the dysfunction of each protein involved in transducing the signal. These discoveries provide evidence that mechanisms to decrease ATR and increase ATM would be effective therapeutic agents.
Figure 1: This diagram from Espach et. al. shows the many chemical pathways that ATM affects.
References
Bin-Bing S. Zhou., and Elledge, Stephen J. “The DNA Damage Response: Putting Checkpoints in Perspective.” Nature 408.6811 (2000): 433-39.
Espach, Y., Lochner, A., Strijdom, H. “ATM Protein Kinase Signaling, Type 2 Diabetes and Cardiovascular Disease.” Cardiovascular Drugs and Therapy 29.1 (2015): 51-58.
Fokas, E., R. Prevo, E. M. Hammond, T. B. Brunner, W. G. McKenna, and R. J. Muschel. “Targeting ATR in DNA Damage Response and Cancer Therapeutics.” Cancer Treatment Reviews 40.1 (2014): 109-117.