By Briga Mullin, Biochemistry and Molecular Biology, ’15
What do a smoker, a two week old embryo, a child with a broken wrist, and a metastatic tumor all have in common? While these are a diverse group of conditions, they all have cells that are experiencing the same process known as epithelial-mesenchymal transition (EMT). Mesenchymal cells are non-polarized, mobile, invasive, and their main function is to secrete extracellular matrix. In contrast, epithelial cells form our skin and the linings of our internal organs. They are normally polarized which means they have a directional structure and are uniformly oriented and are attached to a membrane to form a layer of epithelial tissue. Under certain conditions an EMT will occur and epithelial cells will change their transcription patterns, produce new proteins, destroy the basal membrane they are attached to, and totally convert their phenotype to become motile mesenchymal cells. EMT can be triggered by a variety of conditions and can yield very beneficial or extremely detrimental results depending on the circumstances.
The idea of EMT is fascinating because cellular development is usually thought of as moving from simple towards more differentiated. However, EMT is just the opposite of that. The orderly tissue layer of epithelial cells degenerates into simple undifferentiated mesenchymal cells. It is also worth noting that this process can occur in reverse with mesenchymal cells converting to epithelial cells. This process is known as mesenchymal epithelial transition (MET). In MET, cells differentiate to form more complex structure, which is a more intuitive process than EMT. There are cases where cells can perform multiple ETMs and METs, changing their phenotype back and forth, demonstrating a highly plastic nature .
EMT was first discovered in developing embryos, where a high level of plasticity is necessary. In our two week old embryo, the three germ layers, . Parts of the ectoderm undergo EMT to eventually become endoderm and mesoderm. Later on, EMT is also essential for the development of neural crest cells from neural ectoderm. Thinking about all the changes and developments that go into converting an embryo to a full formed organism, it seems reasonable that there are mechanisms in place to drastically change cell structure and function. This class of EMT, known as type I, is completely essential for all development. However, not all instances of EMT are so straightforward .
The smoker and the child with a broken wrist are both experiencing the same form of EMT known as type II EMT, which is caused by irritation and inflammation . When activated by injury or irritation, fibroblast cells that produce extracellular matrix and bone marrow release molecules that can trigger EMT in neighboring epithelial cells by degrading the basal membrane. This is another example of a situation where EMT is very useful. When there is damage to tissues, EMT creates more mesenchymal cells to secrete growth factors and extracellular matrix, which are necessary to heal damage. However, if inflammation and irritation are caused by a long term stressor such as smoking, too many cells activate an EMT program for too long. Chronic obstructive pulmonary disease (COPD), is a condition where airflow is limited because scarring and swelling in the narrow branches of the lungs make it hard for air to reach sites for gas exchange. The primary cause of COPD is smoking and the mechanisms by which the lungs are affected include EMT induced by cigarette smoke and production of ECM by fibroblasts. Epithelial cells in bronchioles and alveoli experience EMT, and the newly created mesenchymal cells produce excess collagen thickening and hardening the lungs.
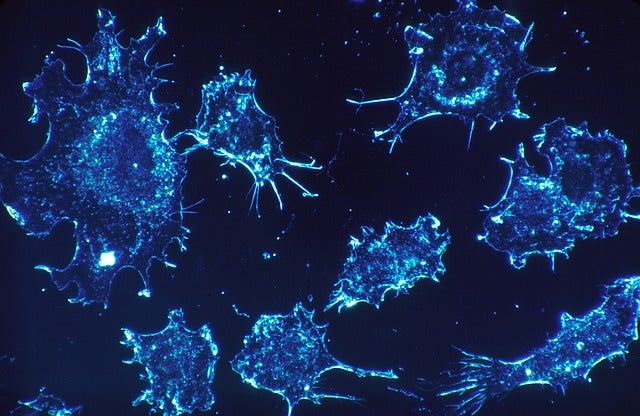
While fibrosis in the lungs or other organs due to type II EMT has serious consequences, the metastatic tumor is the most dangerous example of EMT. When an cancer of the epithelial cells, known as carcinoma, spreads to another area of the body, the key mechanism for the migration of tumor cells is type III EMT. When epithelial tumor cells undergo an EMT, they become motile and invasive mesenchymal tumor cells. If these cells spread throughout the body and successfully colonize new tissues, the primary tumor has become metastatic, and the cancer is significantly more dangerous and difficult to treat.
The process of EMT and its many applications in the body are proof that at all stages of life cellular differentiation has some flexibility. Clearly, this has benefits and drawbacks depending on the scenario. It is appears contradictory that the process of EMT is absolutely necessary for a zygote to develop and grow, but also creates a deadly cancer. Hopefully by furthering the research on the triggers that cause EMT and MET, we can better understand and control this process . Current research includes looking at micro RNAs to regulate cells undergoing EMT and, determining environmental conditions, such as signals sent from neighboring cells, that can induce EMT.
Refrences
Andriani, Francesca et. al. Abstract 4867: Microenvironment stimuli elicited by fibroblasts contribute to epithelial mesenchymal transition and acquisition of stemness phenotype in lung cancer. Cancer Res October 1, 2014 74:4867; doi:10.1158/1538-7445.AM2014-4867
Eurlings IMJ, Reynaert NL, van den Beucken T, Gosker HR, de Theije CC, et al. (2014) Cigarette Smoke Extract Induces a Phenotypic Shift in Epithelial Cells; Involvement of HIF1α in Mesenchymal Transition. PLoS ONE 9(10): e107757. doi: 10.1371/journal.pone.0107757
Kalluri, Raghu and Weinberg, Robert A.. (2009) The Basics of Epithelial-Mesenchymal transition.J Clin Invest.2009; 119(6): 1420-1428. Doi: 10.1172/JCI39104